Preparation for intraoperative navigation
1. Introduction
The use of intraoperative navigation requires that the patient's anatomy and spacial orientation is "registered" with the navigation system. Patient registration is a process whereby fiducial markers are used to precisely define the patient's three dimensional location in space.
Hardware
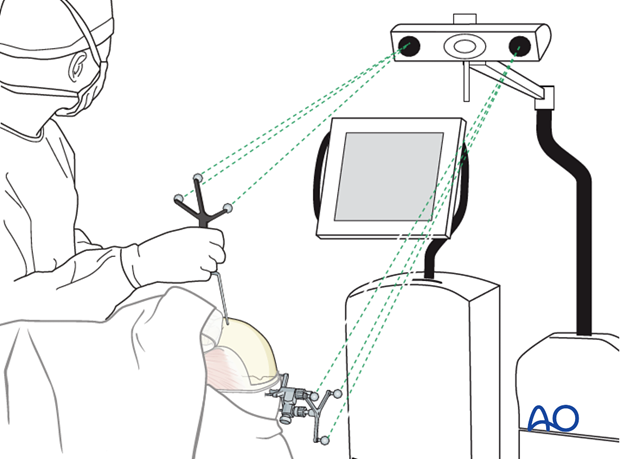
Intraoperative navigation hardware is comprised of three basic components:
- Navigation system
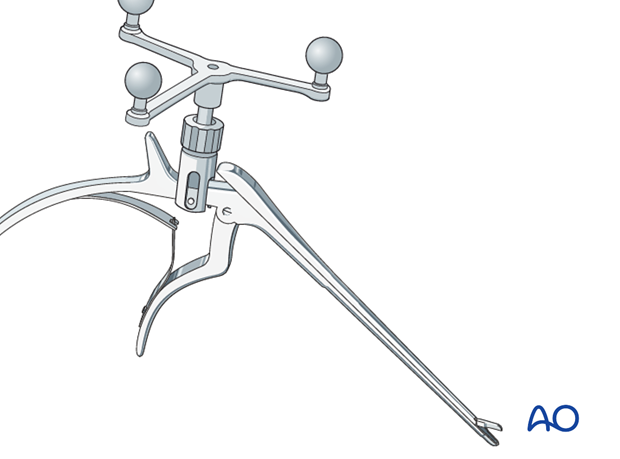
- Skull reference array
- Trackable instrumentation
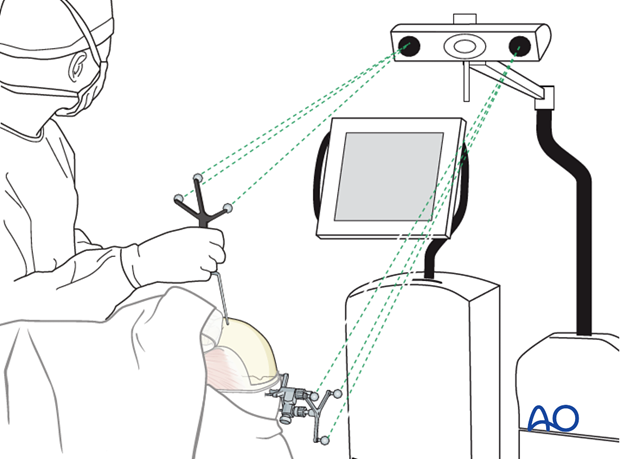
The navigation system consists of a computer, monitor and an infrared digitizer camera. The digitizer camera emits infrared light which is reflected off the skull reference and instrument arrays. The navigation system then triangulates the exact location of the reference arrays in space. There must be a direct line of sight between the digitizer camera and the reference arrays during registration and navigation.
The skull reference array is used to determine the patient's 3D orientation in space. However, the patient's orientation cannot be determined until the registration process is completed.
While there are variations in navigation probe design, the relationship between the infrared reflectors and the tip of the navigation probe is rigidly defined. This allows navigation system to track the tip of the instrument in space with approximately 1 mm accuracy.
2. Registration hardware
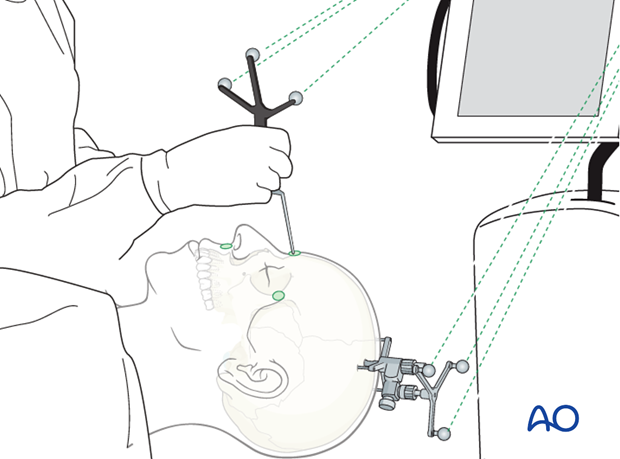
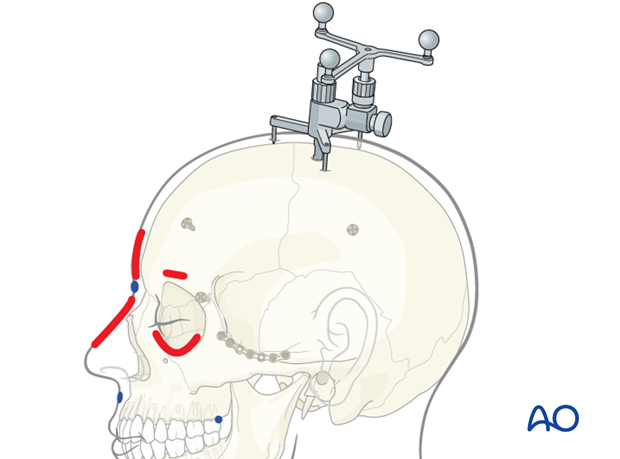
A skull post is applied to the cranium with a central fixation screw.
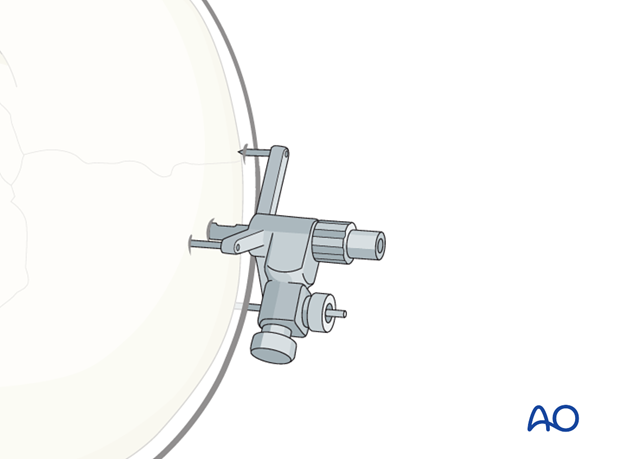
The dynamic reference frame (DRF) is then attached to the skull post. The DRF will be used to define the patient's 3D orientation in space.
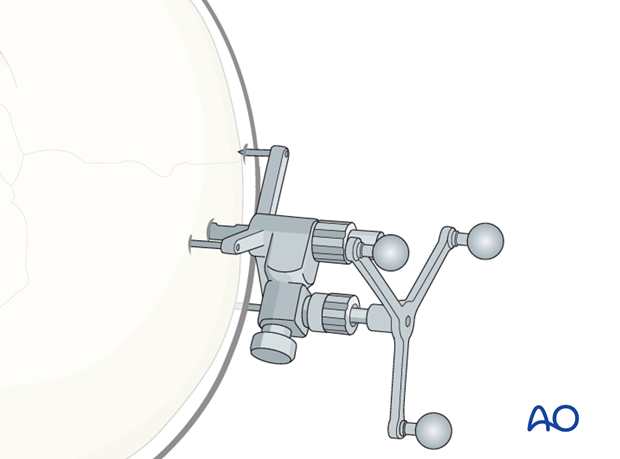
The rigid screw fixation maintains the relationship between the patient and the DRF during the registration process and surgical procedure.
At this point the tip of probe as well as the DRF are defined in all three dimensions.
Patients anatomy is also clearly defined in three dimensions within the navigation system, however the patients three-dimensional orientation has not yet been defined within the navigation system.
The registration process will define the patient's orientation in space relative to the DRF.
3. Patient registration
There are several techniques used for patient registration. These will be discussed in more detail below. A basic example is presented to demonstrate the underlying principles.
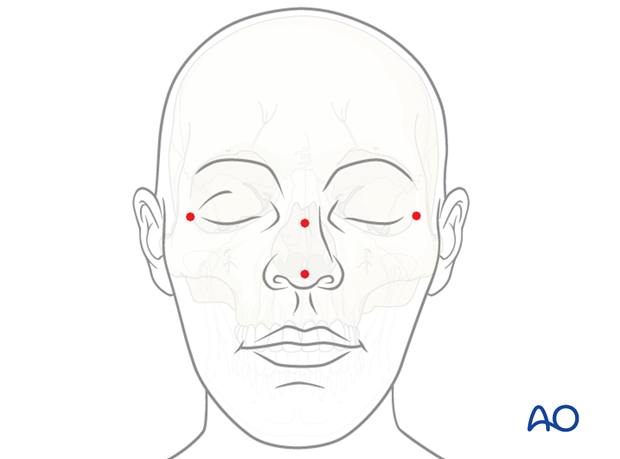
A minimum of four fiducials are defined on the virtual patient.
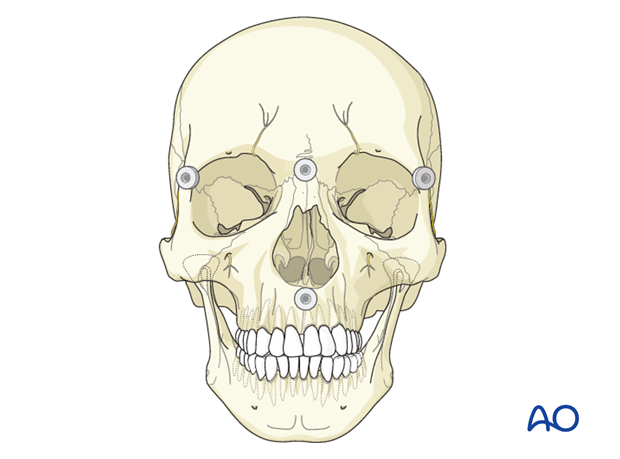
The tip of the navigation probe is sequentially placed on each point. The navigation system uses these anatomical landmarks to triangulate the position of the physical patient in space relative to the DRF.
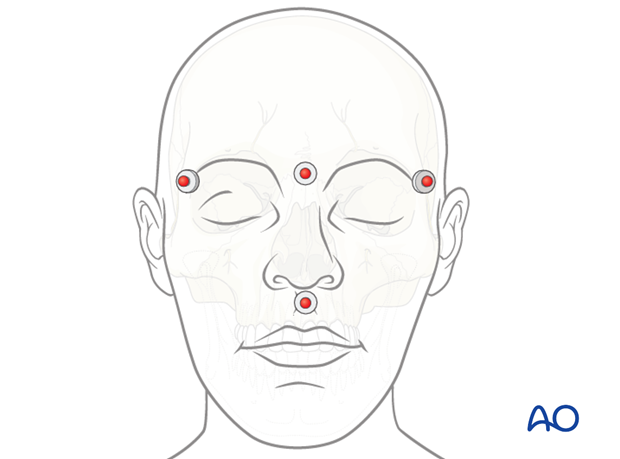
Independent of the registration strategy used, there are four basic principles for optimal fiducial placement. The greatest accuracy will be achieved by
- Using a maximal number of fiducial points.
- Separating the fiducials with the largest possible distance on the skull/skin.
- Placement of the surgical field at the center of the fiducial markers.
- Not placing the fiducials in a single line or a single plane.
Skin surface registration
Skin surface registration is commonly performed by moving a registration laser pointer or navigation probe over the surface of the skin. This accumulates large number of fiducials for patient registration.
Alternatively, skin surface registration strategies include the use of anatomic landmarks already present on the patients or...
...by placement of fiducial markers on the skin prior to acquisition of the CT dataset used for planning/surgery.
This technique offers the ability to obtain a maximal number of fiducial landmarks dispersed over the largest volume surrounding the surgical area of interest. It also limits radiation exposure by allowing the surgeon to use CT data in which fiducials are already present.
This technique is primarily used for secondary corrections when no tissue edema is present. Any change in surface contour (resolution of posttraumatic edema) will result in inaccuracies or inability to register the patient. In the author's experience, procedures performed greater than 24 – 48 hours after CT acquisition will not provide an accurate registration. In these cases a current CT would need to be obtained.
Intraoperative re-registration with skin surface landmarks is not possible.
Bony landmarks
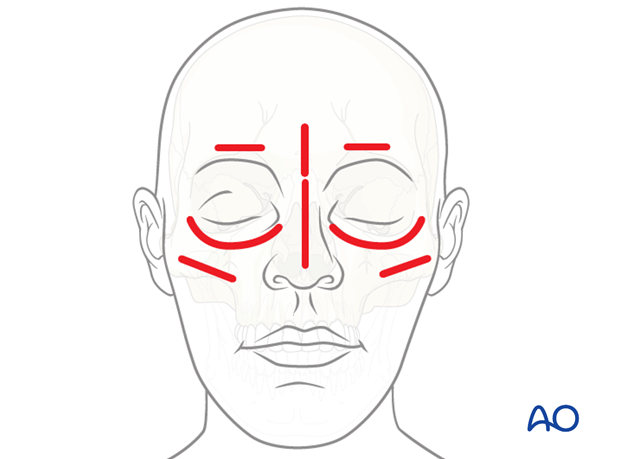
Bone surface registration is performed by moving the navigation probe between defined landmarks on the skull surface. These landmarks must be defined on the virtual patient during the presurgical planning process. These fiducials may include anatomic landmarks (ie, suture lines or bone prominences/concavities, teeth etc.).
If necessary during registration, the probe is passed through the skin so it may be placed directly onto the bone surface.
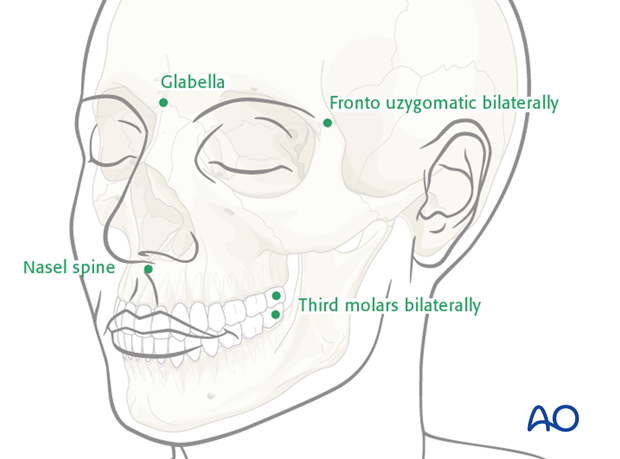
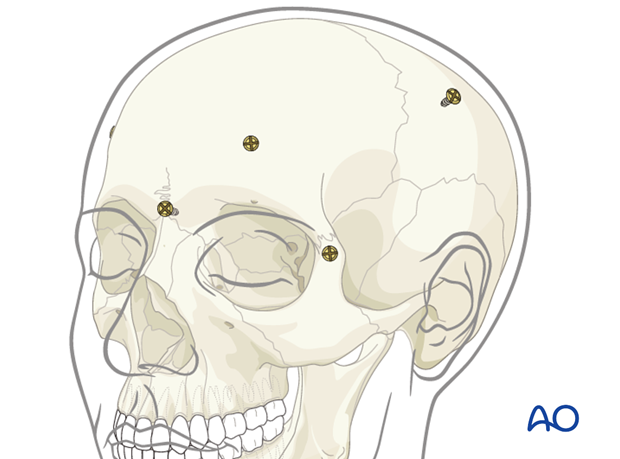
The surgeon may place bone screws in non mobile segments of the skull or use previously placed hardware as fiducials for registration.
If bone screws are used, a repeat CT scan of the patient with the screws in place will be necessary. As with atomical bony landmarks, these fiducials must be defined on the virtual patient during the presurgical planning process.
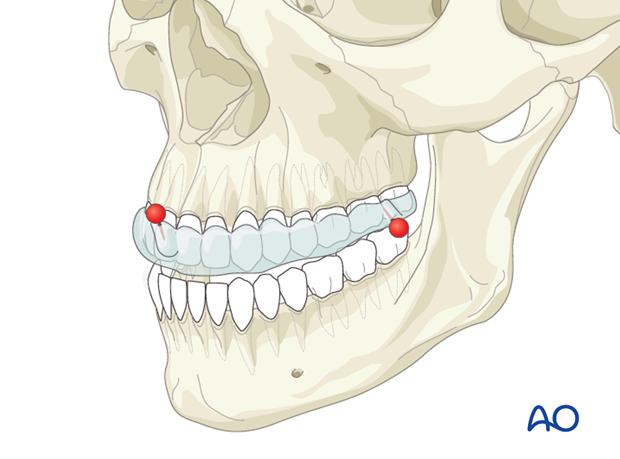
Oral appliances
In dentate patients with an un-injured maxilla, a splint containing fiducial markers can be fabricated to fit onto the patient's maxillary dentition.
It is necessary to obtain a CT scan with the splint in place. The fiducials on the virtual splint may then be defined during the presurgical planning process.
The splint may be removed and replaced intraoperatively for use in registration.
4. Backup plan
In the event of difficulties during registration, a prudent registration plan should include a primary and secondary registration technique.
For example, a surgeon using skin surface registration should place virtual anatomic bony landmarks which can be used should the skin surface registration fail.
Similarly a surgeon using an oral appliance should consider placing bony anatomic landmarks in the event that the appliance is unavailable or not adequate for registration.
A final backup strategy is intraoperative registration, which can be used if the DRF is dislodged from the skull. Intraoperative registration is performed by defining four or more anatomic landmarks (drill holes, ink marks, or screws) on the skull after the initial registration has been completed.
Should the skull reference become dislodged during the procedure, these intraoperative landmarks can then be used to re-register the patient after the skull reference array is reapplied.
5. Registration of equipment
All surgical instruments can be registered by attaching a DRF to them via a clamp.