Panfacial fractures (sequencing of repair)
1. Introduction
The determination of ideal sequencing of a complex panfacial trauma can be the greatest challenge to a maxillofacial surgeon.
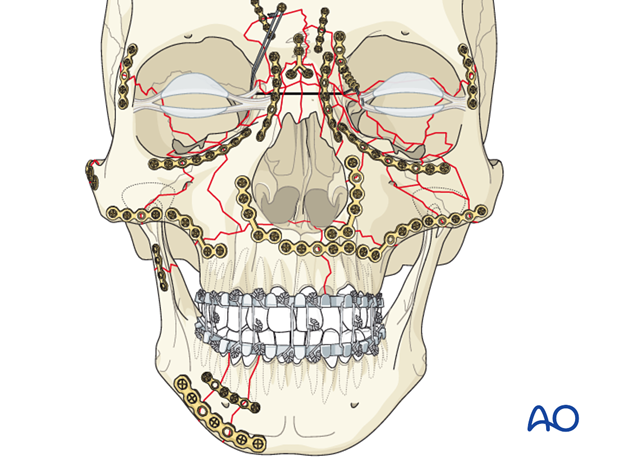
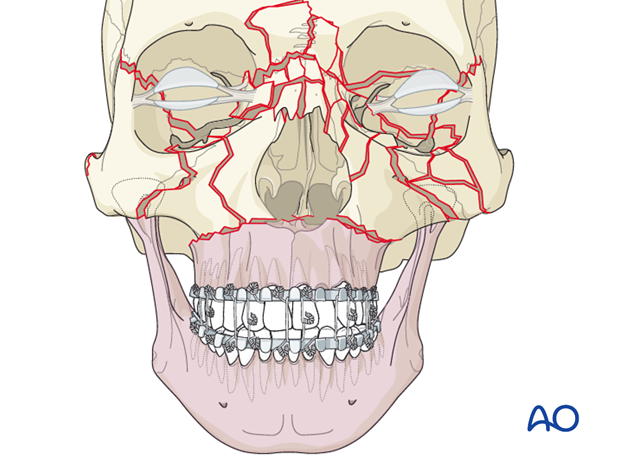
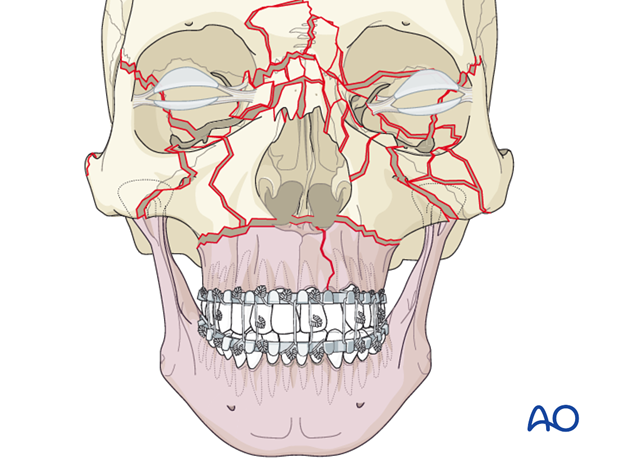
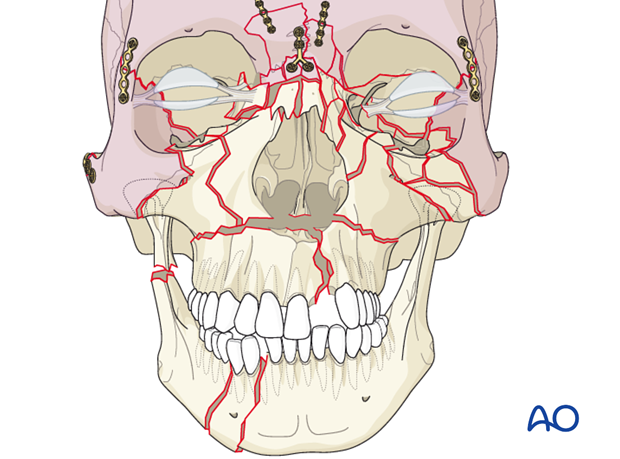
The illustration represents most facial fractures seen frequently.
This represents the following fractures:
- Le Fort I
- Le Fort II
- Le Fort III
- Frontal sinus
- Nasal
- Bilateral NOE
- Bilateral zygoma
- Bilateral orbit including the medial and lateral wall, and orbital floor and roof
- Simple sagittal split of the palate
- Segmental mandibular body/parasymphyseal
- Unilateral fracture of the condylar process.
2. Principles
Goal
The goal is to restore the anatomy in all three dimensions, plating the maxillofacial buttresses wherever necessary.
One of the biggest advancements in the management of panfacial fractures is recent developments in 3-D imaging, mainly in CT and cone beam technology. This allows individual assessment of injuries and is a prerequisite for optimal diagnosis, planning, reduction, and outcome control.
Radiographic evaluation should not be restricted to the 3-D views since multiplanar 2-D view may show critical features not seen in the 3-D views.
The availability of an intraoperative model or skull greatly facilitates proper contouring of hardware and facilitates proper skeletal reconstruction.
Two options for sequencing
There are two options for sequencing:
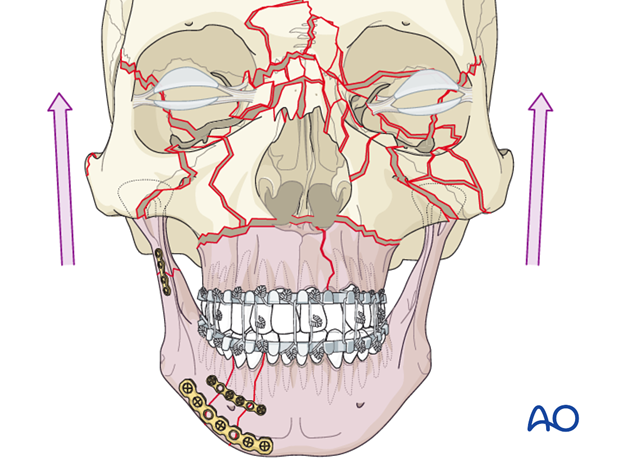
- Re-establish the maxillo-mandibular unit as the first major step of the sequencing (bottom-up).
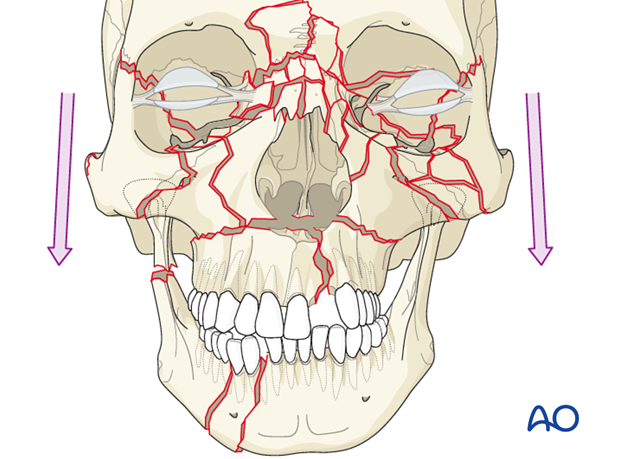
- Starting with the reduction and fixation at the level of the calvarium and working in a caudal direction (top-down).
1) Re-establish the maxillo-mandibular unit as the first major step of the sequencing (bottom-up).
Once the maxillomandibular unit is established, most surgeons start from the calvarium and proceed in a caudal direction with reduction and fixation.
2) Starting with the reduction and fixation at the level of the calvarium and proceed in a caudal direction with reduction and fixation (top-down).
It should be noted that with this second option of sequencing, reestablishment of the proper maxillomandibular unit is still very important, but may be achieved later in the case.
Reestablishing the maxillo-mandibular unit as first priority
In the following description, we focus on the first method of sequencing, reestablishing the maxillomandibular unit as first priority.
The first step is to focus on the reestablishment of the maxillomandibular unit.
Note: If the mandible is going to be used to position the maxilla through MMF, the mandible must be completely reconstructed from one condyle to the other.
If there is a Le Fort type fracture but no sagittal split of the palate and no mandibular fracture, the reestablishment of the maxillomandibular unit should be fairly simple, using arch bars and MMF.
If there is a Le Fort type fracture and no sagittal split of the palate and mandibular fractures, establishment of the correct mandibular dental arch configuration can be obtained using the intact maxillary dental arch through MMF.
Click here for a discussion of multiple mandibular fractures.
If there is a Le Fort type fracture, a sagittal split of the palate, and no mandibular fractures, the mandibular dental arch may be used as a guide in reestablishing the occlusion and width of the maxillary dental arch with placement of arch bars and MMF.
The recommended sequence for this portion of the treatment of the palate is dependent on whether it is a simple or complex (comminuted) palatal fracture.
Click here for a description of open treatment of a simple injury and here for a complex injury.
If there is a Le Fort type fracture and a sagittal split of the palate together with mandibular fractures, reestablishment of the proper width of the disrupted dental arches is more difficult. The surgeon must reconstruct one dental arch and use it as a template for the other.
This can be done one of two ways. The first being anatomic reduction and the second using model surgery and fabrication of splints on dental casts.
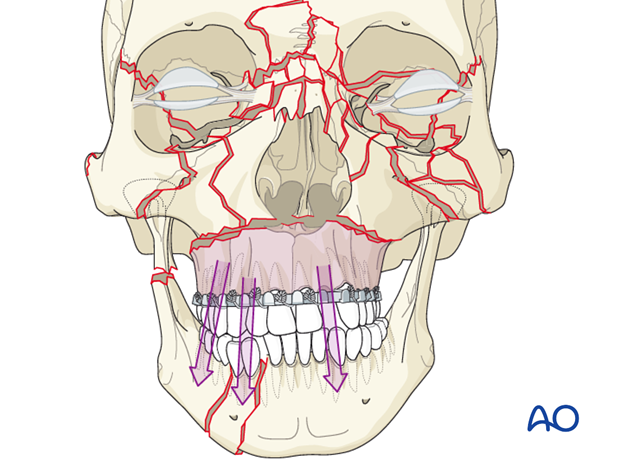
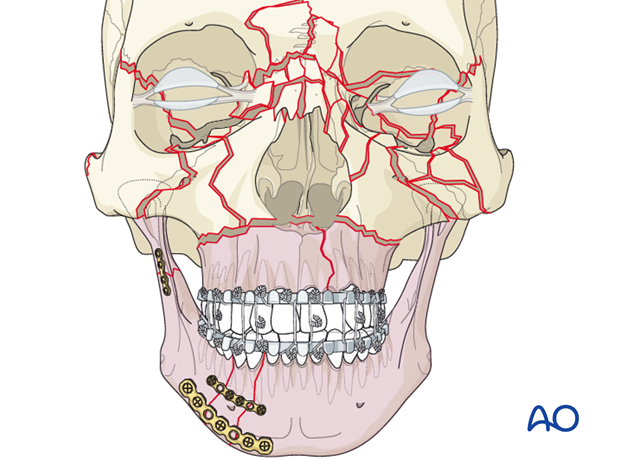
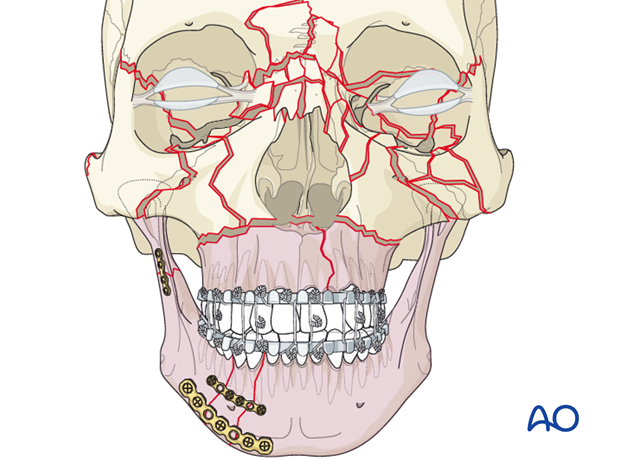
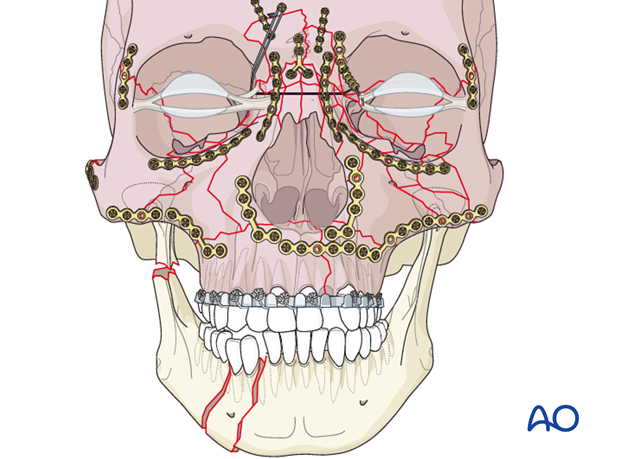
In the illustration, the mandible was anatomically reconstructed and used to restore the width of the maxilla through the use of MMF (first option).
Note: If the mandible is to be used to position the maxilla through MMF, the mandible must be completely reconstructed from one condyle to the other.
The second option involves taking dental impressions, making dental models, and from these models, performing model surgery to examine and reestablish the premorbid occlusion.
In these complex cases, cuts need to be made in the maxillary portion and the mandibular portion of the dental models to recreate the fractures to determine the premorbid occlusion and contour of the maxillary and mandibular arches.
Once the maxillary and mandibular model surgery has been performed, palatal and/or mandibular splints are fabricated for use during surgery.
This technique may also be considered in any case where either the palatal fracture or mandibular fracture is very complicated but the other portion of the maxillomandibular unit is intact. The surgeon may choose to use dental impressions and models with any complex fracture involving the dentition where proper premorbid occlusion is uncertain.
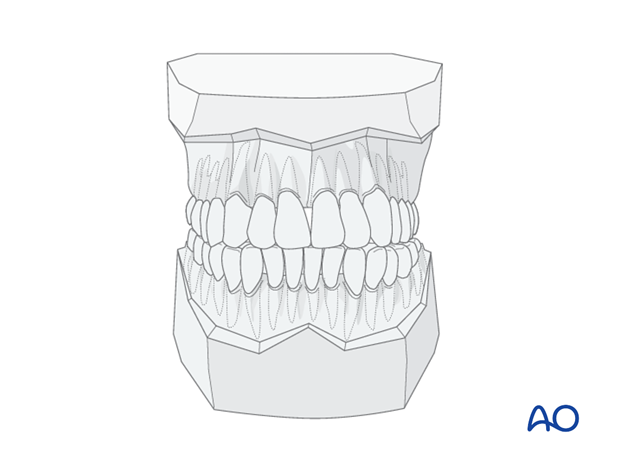
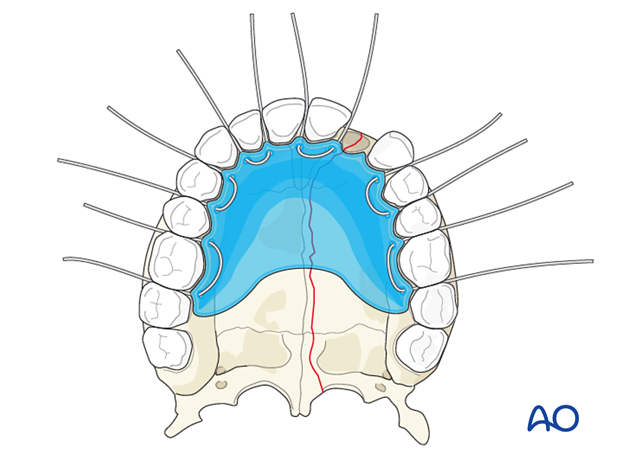
This is an example of a palatal splint that has been prefabricated after model surgery. Circumdental wires are ligated to the arch bars to restore the maxillary arch form.
If a mandibular lingual splint is needed, it is fabricated and fixed to the mandible, also using arch bars and wires.
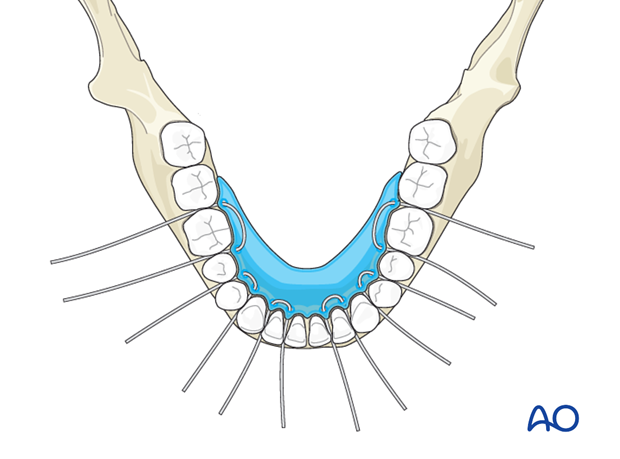
This is an example of a lingual mandibular splint that has been prefabricated after model surgery. Circumdental wires are ligated to the arch bars to restore the mandibular arch form.
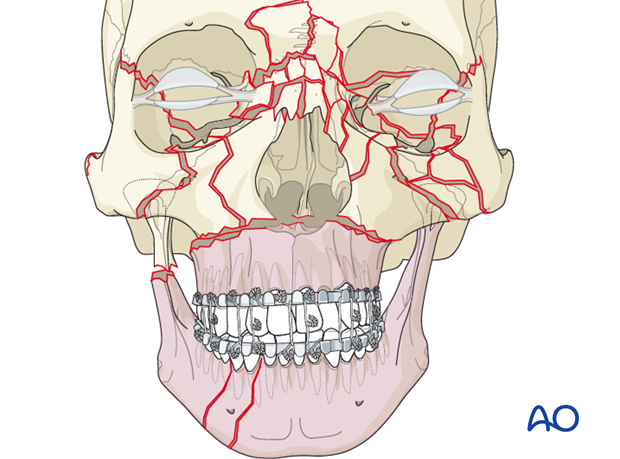
In cases where there are condylar fractures, open treatment of these fractures will restore proper mandibular height and chin position.
In this illustration the mandible was reduced and fixed and then used as a guide for the reduction of the palate.
Note: If the mandible is to be used to position the maxilla through MMF, the mandible must be completely reconstructed from one condyle to the other.
Summary
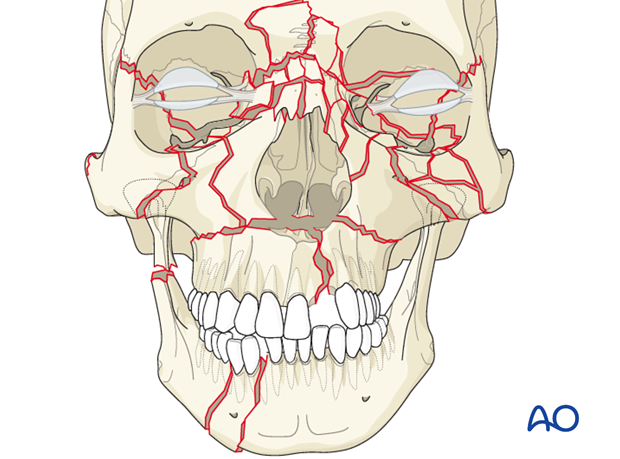
With a combination of the modalities described the proper maxillomandibular unit has been restored with the proper premorbid occlusion.
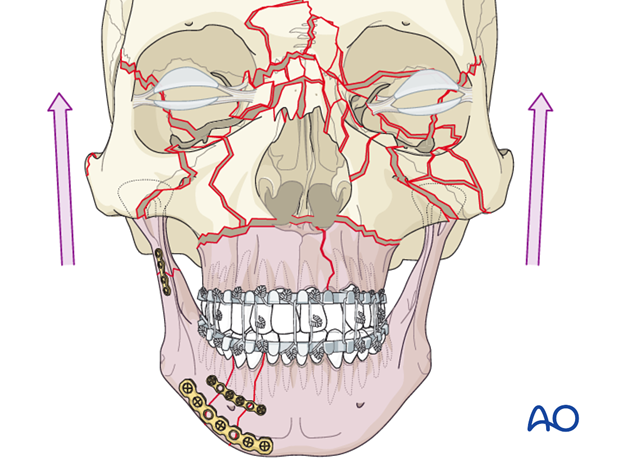
The next step is to begin the reduction and fixation of the remainder of the midface starting from the calvarium and working in a caudal direction. (Refer to top-down procedure for details).
3. Sequencing from the calvarium down
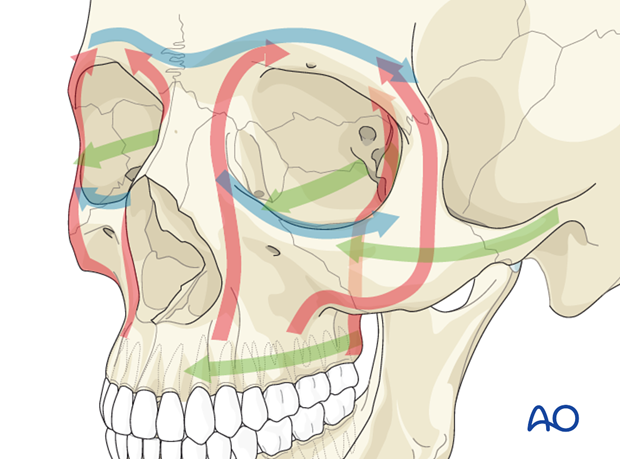
The reconstruction sequence to reestablish midfacial pillars (buttresses) and dimensions starts with the most reliable reference structures and on the side with the least comminution.
The first priority is to address any significant calvarial, frontal sinus, and orbital roof fractures. Using the calvarium as the foundation for the remainder of the midface reconstruction, the surgeon progresses from this level down to the Le Fort I level. The fractures at the Le Fort I level are the second to last fractures to be plated.
The zygoma is positioned into its proper three-dimensional position taking care to properly line up the lateral wall of the orbit with the greater wing of the sphenoid.
Click here for description of fracture fixation of zygomatic complex fractures.
The proper alignment of the zygomatic arch and the infraorbital rim must be taken into consideration during the reduction of the various fractures.
The completion of the reconstruction of the periorbital areas is performed by addressing the NOE and nasal fractures.
Note: Where reconstruction of the medial canthal tendon is necessary it is the final step before wound closure.
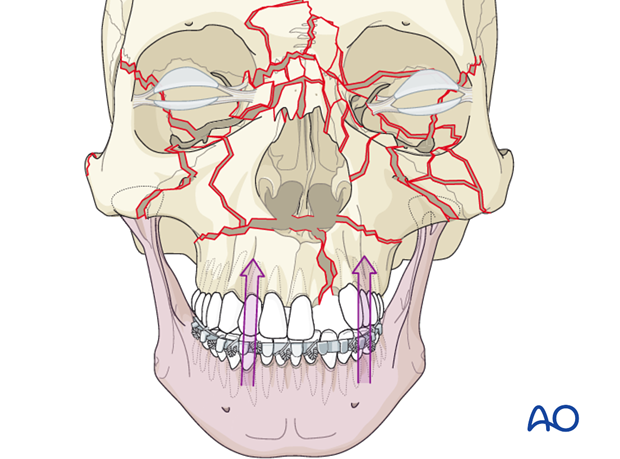
The next step in midface reconstruction is fixation across the Le Fort I level.
If everything has been perfectly aligned, the fractures at the Le Fort I level should also align perfectly. If a patient has a malalignment at the Le Fort I level, the surgeon needs to reassess the other fracture alignments, and consider a correction.
From an esthetic standpoint, a minimal malalignment at the Le Fort I level is not as noticeable as a malalignment of the orbits. The surgeon needs to decide whether the malalignment at the Le Fort I level will be associated with occlusal problems.
The last fractures to be reconstructed are generally the fractures of the orbital walls and orbital floor.
Maxillomandibular fixation is now performed and the mandibular fractures are repaired.
Any condylar fractures may be treated open or closed depending on the wish of the surgeon.
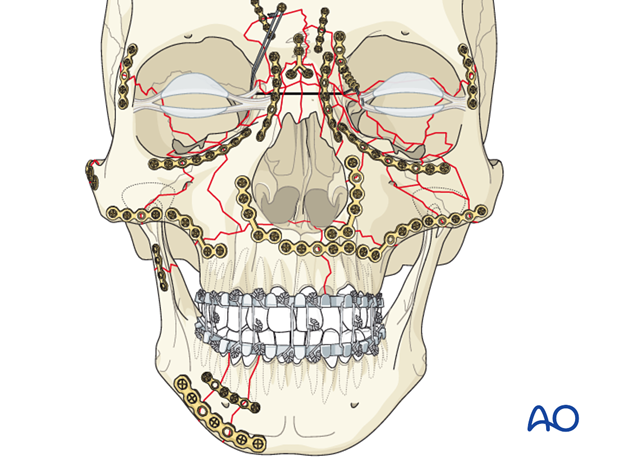
The occlusion should be rechecked at the end of the case. Depending on the fixation and stability of the fractures, the comminution and complexity of the case, and the presence of an untreated condylar fracture, the surgeon needs to decide whether to leave the patient in MMF or not.
4. Follow-up and potential complications
A panfacial fracture in particular should have good postoperative radiologic documentation of a proper reduction. Rescanning for assessing pneumatization and contour stability should be considered depending on the nature of trauma.
Panfacial fracture patients need follow up which is appropriately coordinated by the CMF surgeon.
Dynamic forces (eg, masticatory function and occlusion), scarring, edema, sensory and motor dysfunction, atrophy, temporomandibular joint (TMJ) dysfunction, dental problems, mucoceles may contribute to unfavorable esthetic and functional outcome with secondary deformity.












