Retrobulbar hemmorage
1. Retrobulbar Hemorrhage - Compartment Syndrome in the Orbit
Postoperative bleeding within the orbit can result in retrobulbar hemorrhage (ischemic and/or compressive optic neuropathy) and blindness.
Detailed postoperative monitoring of vision with documentation is highly recommended.
The clinical personnel looking after the patient must be familiar with the typical signs and symptoms of a retrobulbar hemorrhage.
The patients head should be elevated postoperatively (30°-45°).
The use of a small drain may prevent the occurrence of a sub-periorbital hematoma.
Subperiosteal orbital hemorrhage and compartmentalization of blood within the septal pockets (of the extra or intraconal space) may result in elevation of the orbital tissue pressure. This in turn may lead to decreased vascular perfusion and ischemia of the optic nerve or the retina with visual loss as the most ominous complication.
During the dissection, meticulous hemostasis must be assured to prevent postoperative bleeding. A bloodless field is rechecked at the end of the intraorbital procedure prior to closure.
Postoperatively the vision must be monitored regularly.
The signs and symptoms of a retrobulbar hematoma may include:
- Painful Proptosis
- Increased orbital tissue tension, increased intraocular pressure
- Ecchymosis of eyelids
- Chemosis
- Decreased Visual Field
- Decreased Visual Acuity/Loss of Vision
- Afferent Pupillary Defect (APD in swinging flash light test)
If circumstances do not dictate an emergent intervention, CT or MRI imaging greatly aids in the identification of the location and extent of the hemorrhage in order to plan the decompression and evacuation.
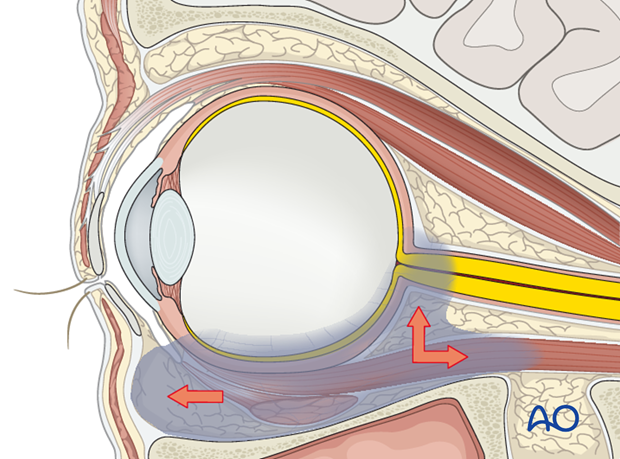
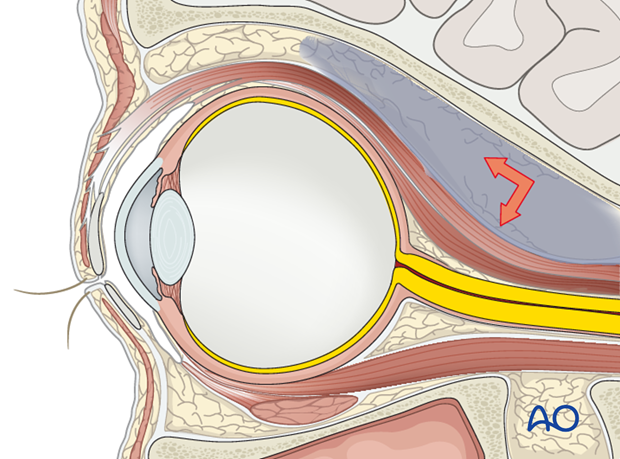
The surgical procedure can be differentiated in an extraconal hematoma of the superior orbit in contrast to a hemorrhage involving the extra- and intraconal compartments in the lower circumference of the anterior and midorbit regions as shown in the previous illustration.
Vision treatment requires prompt intervention with immediate decompression of the expanding hematoma by dissection of the lateral canthus (lateral canthotomy) and disinsertion of at least the inferior crus of the lateral canthal tendon (inferior cantholysis). This will allow for the globe to prolapse anteriorly relieving the pressure within the orbit.
Confined subperiosteal blood collections may necessitate surgical evacuation under direct vision and even decompression of the bony cavity.
Mega dose systemic corticosteroid treatment and osmotic agents are also part of established protocols for the treatment of this condition.












