Cranioplasty (bone versus alloplast)
1. Indications
Cranioplasty refers to the procedure of recreating the solid covering of the skull that protects the brain from injury. It is also important to give the patient a normal appearance.
Cranioplasty is indicated for the repair of defects in the cranial vault. Small defects are created whenever a burr hole is made. These are of course non problematic and are generally covered with burr hole cover plates. However, traumatic injuries may result in significant loss of bone. There are also situations in which a cranial bone flap is not replaced leaving a significant defect. Infection in a bone flap will require debridement and therefore also leave a significant defect.
Patients are often required to wear helmets to protect them from further injury during the time that the dura lacks a solid protective covering.
2. Technique
Various materials are available for performing cranioplasty.
Autogenous
While autogenous bone is an excellent match and is the only material that will be vascularized (with the exception of replacing a saved bone flap), it will require a donor site. Harvesting bone from a donor site adds time and potential morbidity to the procedure. There is also a risk of resorption of the grafted bone.
Donor site options include split calvarium from another portion of the skull. Some surgeons have used split rib because of its natural curvature and the ability to shape it.
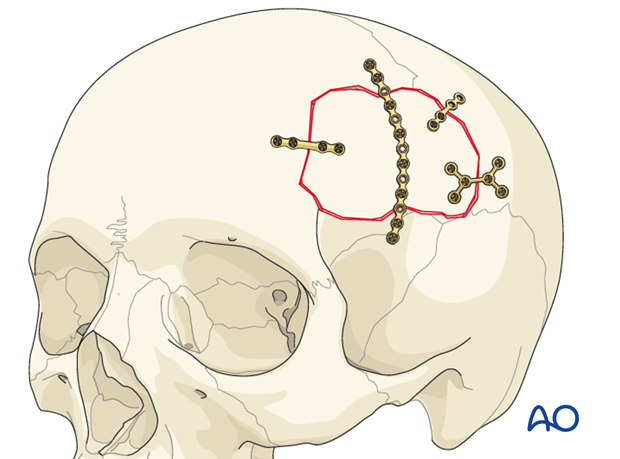
When bone is used in cranioplasty, it must be rigidly fixed to minimize resorption. The junction between the native bone and the graft requires a non load-bearing repair, therefore, small thin plates and short self-drilling screws can be used to avoid the risk of penetrating the dura. Depending on the geometry of the defect, typically 3 small plates will stabilize the reconstruction, though sometimes more may be necessary.
Alloplastic
Numerous materials have been used to repair skull defects.
- Prefabricated/custom-made (patient specific) implants
With the development of sophisticated modern technology, it is now possible to utilize the data from high resolution CT scans to precisely recreate the defect that we wish to repair on a computer generated model. This allows for creation of a custom-made implant to precisely fit the defect. Depending upon the system used, a variety of implant materials may be utilized. These implants will have small overhangs that can be fixed to the surrounding bone...
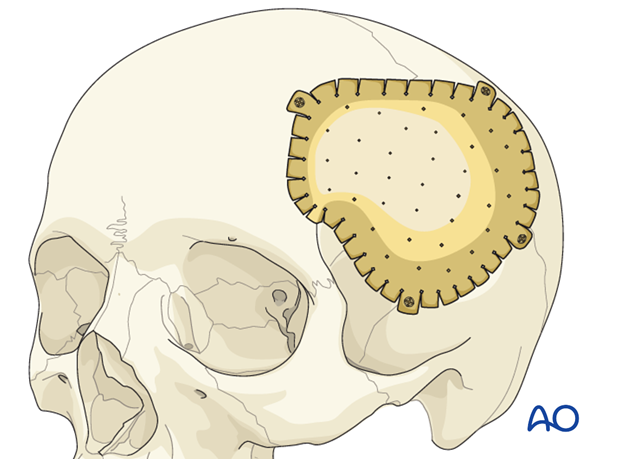
...or they may just lay into the defect requiring stabilization with plates.
Note: some implant materials such as titanium can not be adjusted in situ while others such as high density porous polyethylene and polymethylmethacrylate can be altered with a drill at the time of implantation.
- Polymethylmethacrylate cement (PMMA, mixed soft and molded)
The powder and the liquid components are mixed into a thick paste which is laid over the dura with a spatula and then molded to precisely fit the defect. The surface is molded to match the contour of the normal skull.
Note that the setting of the cement is an extremely exothermic reaction, and the cement can actually become too hot. Neurosurgeons worry about the potential damage to the underlying brain parenchyma leading to seizures and prefer to remove the implant and to allow it to harden outside of the patient.
Care should be exercised to minimize inhalation of the fumes.
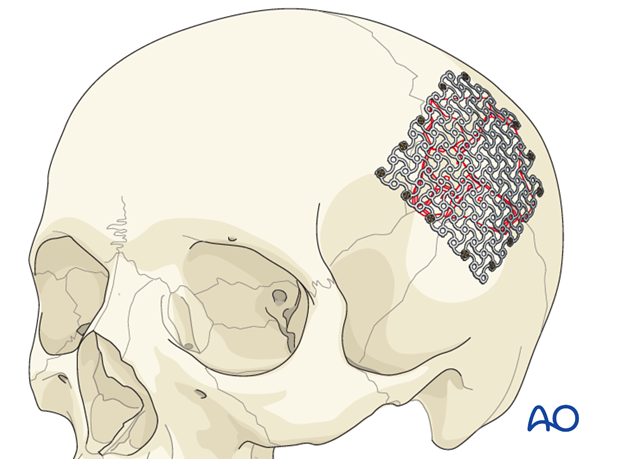
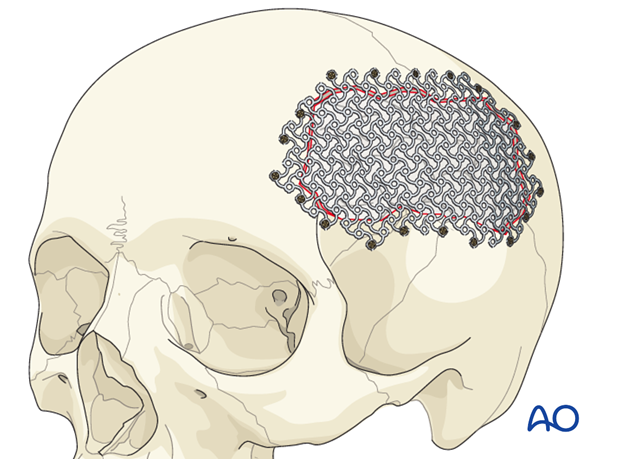
- Titanium mesh
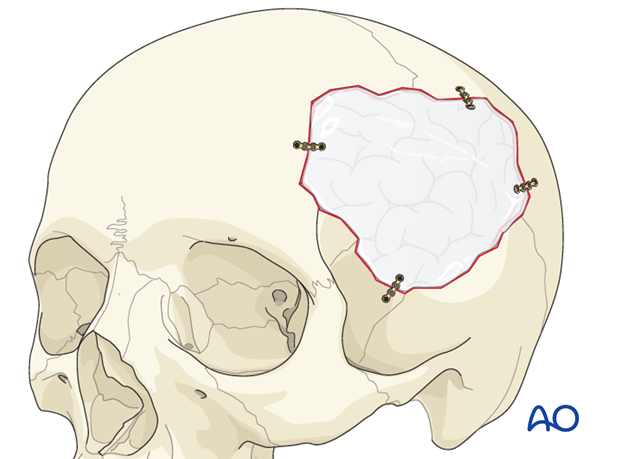
Depending upon the size of the defect titanium mesh may be used alone as the sole method of repair or it may be combined with a hydroxyapatite cement to create more structure and better contour.
When used alone, the appropriate mesh is selected and cut so that it will extend at least 1 cm beyond the actual defect on all sides. It is then fixed in place circumferentially with enough screws to ensure stability.
For use with hydroxyapatite cement see below.
One of the disadvantages of using titanium is the artefact it causes during MRI and CT scans.
- Hydroxyapatite (HA) cement
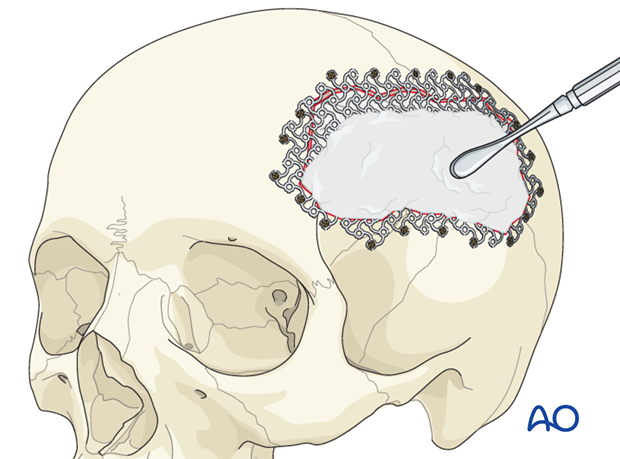
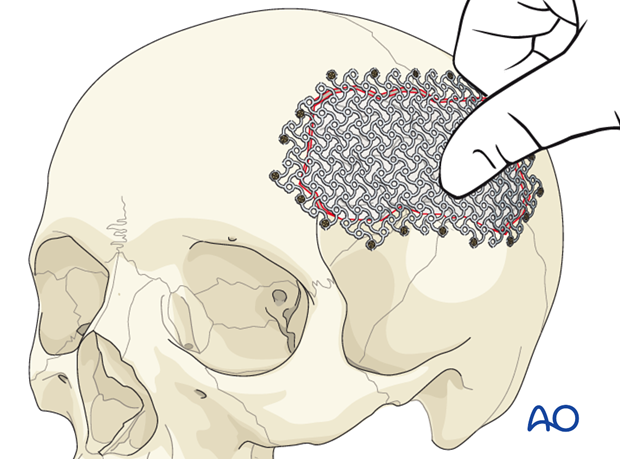
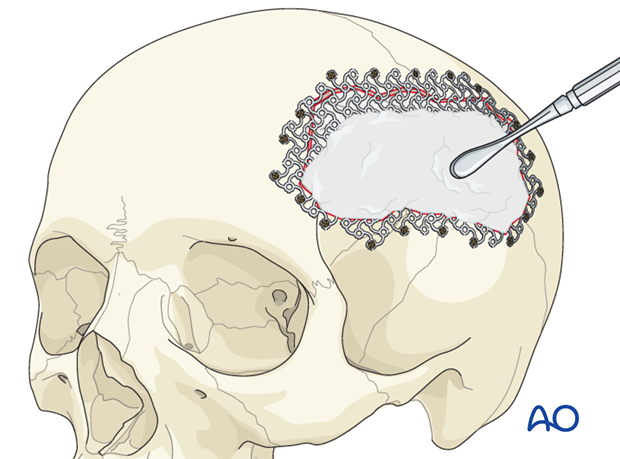
Some surgeons will use HA cement alone for repair of small defects. Others prefer to use the HA cement in combination with the titanium mesh that is placed into the defect so that it is at the level of the inner table. The residual defect is then filled with HA cement so that it conforms to the shape of the outer table. To perform this, a malleable mesh (3-D mesh) is placed across the defect and fixed with screws around the periphery.
The central portion of the mesh is then pressed into the defect so that its shape corresponds to the natural inner-table position. (If the mesh used does not stretch, then it must be contoured before it is fixed.)
The residual defect can then be filled with HA cement. The cement is mixed until it has a putty-like consistency and then it can be applied over the mesh with a spatula and smoothed to match the contour of the natural skull.
3. Complications (early)
- Hematoma
- Infection
- Screw failure
- Implant breakage
- Failure of HA cement
- Wound breakdown
4. Complications (late)
- Bone graft resorption
- Implant loosening
- Implant extrusion
- Infection
- Seizures












