Neurovascular injuries
1. Neurological injuries
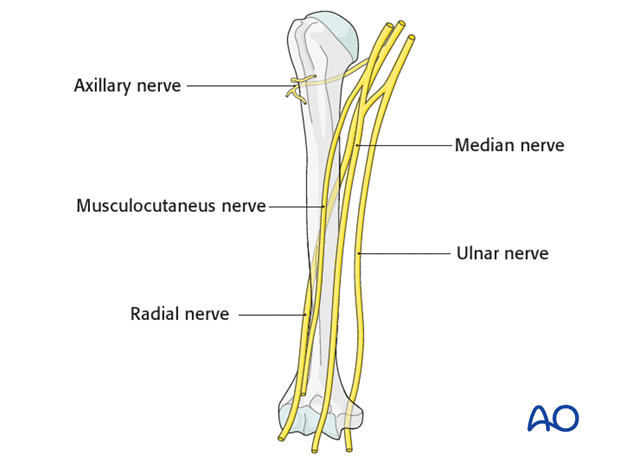
In some situations, humeral shaft fractures can be associated with neurological injuries. Most frequently the radial nerve is affected. Less frequently other nerves are involved:
- Axillary nerve
- Musculocutaneus nerve
- Median nerve
- Ulnar nerve
The likelihood of an additional nerve injury depends on:
- Type of trauma (high- versus low-energy trauma)
- Severity of soft-tissue injury
- Fracture location (ie Holstein-Lewis fracture, illustrated)
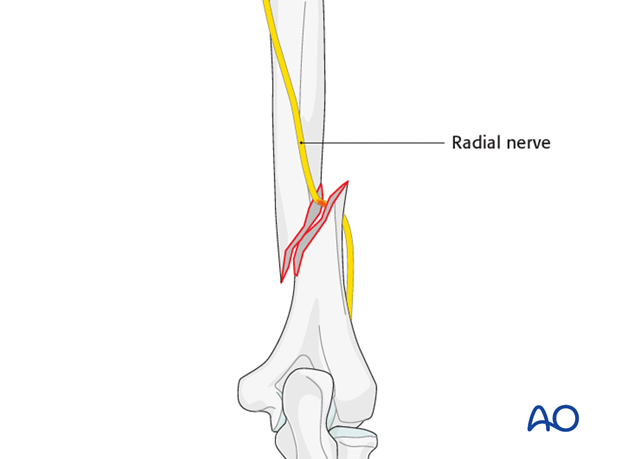
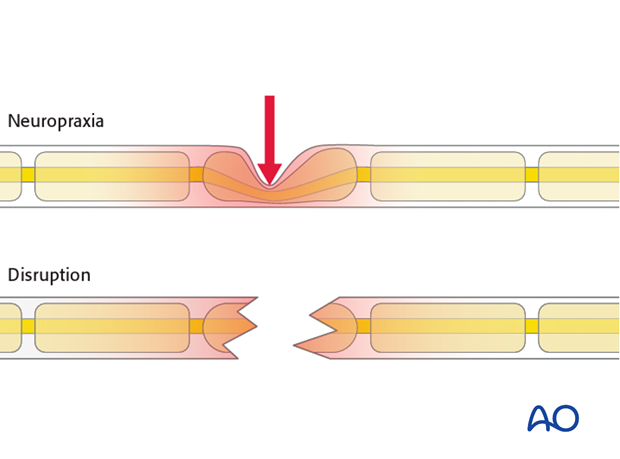
Since many radial nerve lesions recover spontaneously and do not require any surgical treatment, it is important to differentiate between nerve disruption and neurapraxia to decide whether to explore the nerve or not.
Nerve exploration should be considered under the following situations:
- High-energy trauma
- Open fractures
- Holstein-Lewis fractures
- New neurological symptoms after surgical fixation (especially after plating, use of cerclage, application of external fixator using small stab incisions)
When planning nerve exploration, be prepared for neurosurgical procedures such as readaptation or grafting.
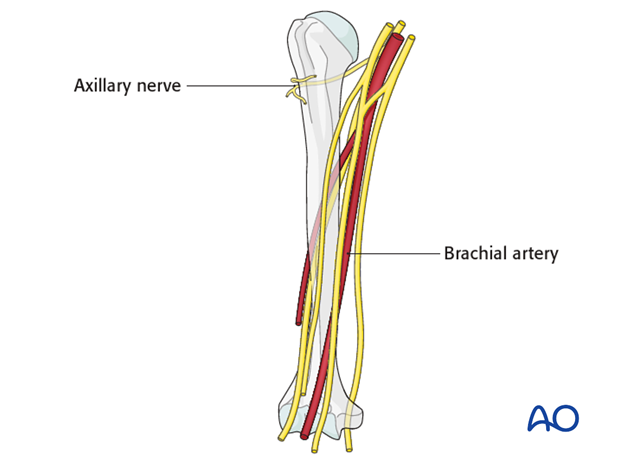
2. Vascular injuries
Humeral shaft fractures may be associated with vascular injuries. Most frequently the brachial artery is affected. Those injuries are emergency cases and require quick and straight forward diagnostics and therapy.
If no peripheral pulses can be detected, further, immediate imaging is mandatory either by arteriography or iv contrast CT scans.
In major vascular injuries, immediate fixation of the fracture with external fixation and additional vascular surgery (eg direct repair or grafting) is the treatment of choice. Definitive fixation using a plate or nail is rarely performed initially. Be aware of perfusion-reperfusion damage and later compartment syndrome.