Bridge plating
1. General considerations
Introduction
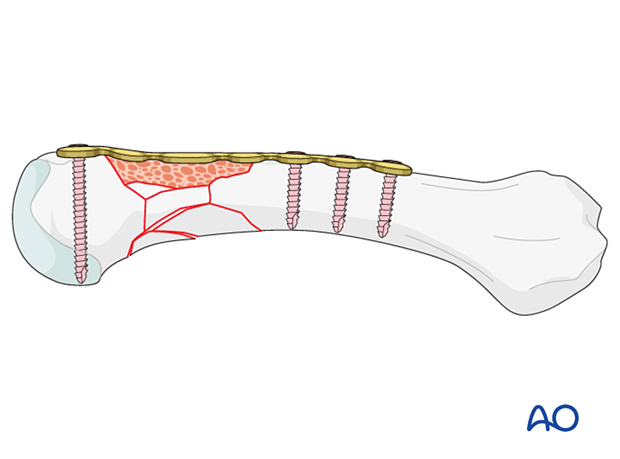
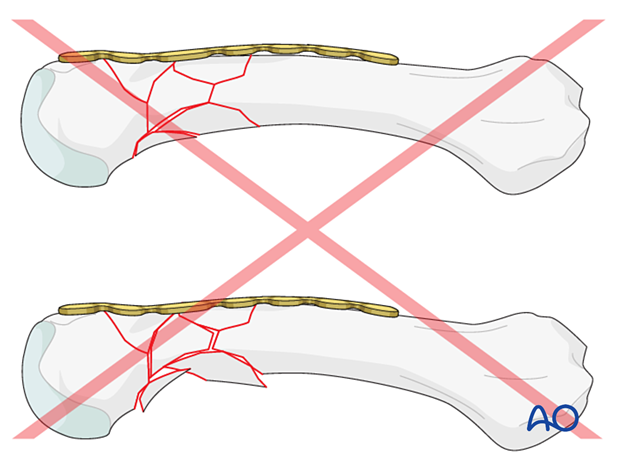
Bridge plating uses the plate as an extramedullary splint fixed to the two main fragments while the complex fracture zone is bridged.
The dissection required for anatomical reduction of all fragments would risk disturbing their blood supply and is not necessary. If the soft-tissue attachments of these fragments are preserved, and the fragments are relatively well aligned, healing is predictable.
It is important to restore axial alignment, length, and correct rotational alignment of the main shaft fragments.
Relative mechanical stability, provided by the bridging plate, leads to healing by callus formation.
Multiple metacarpal fractures
When multiple metacarpals are injured, restoration of length and rotation is difficult. If one of the finger metacarpals is intact, the fixation is started on the adjacent metacarpal and then continued sequentially.
If all four metacarpals are fractured, fixation is started with the least comminuted, and then the adjacent metacarpals are fixed. With one incision, it is possible to fix two metacarpals.
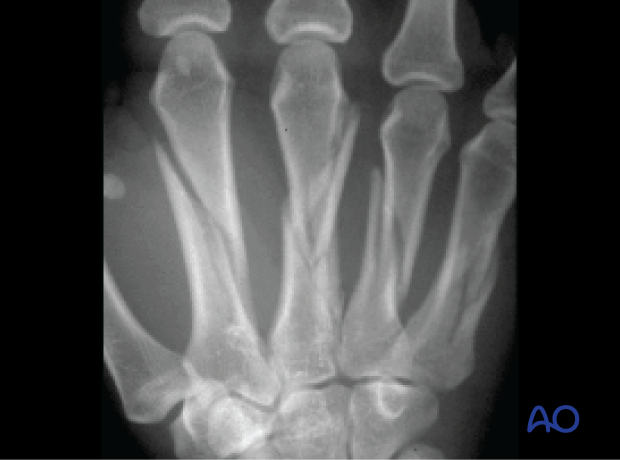
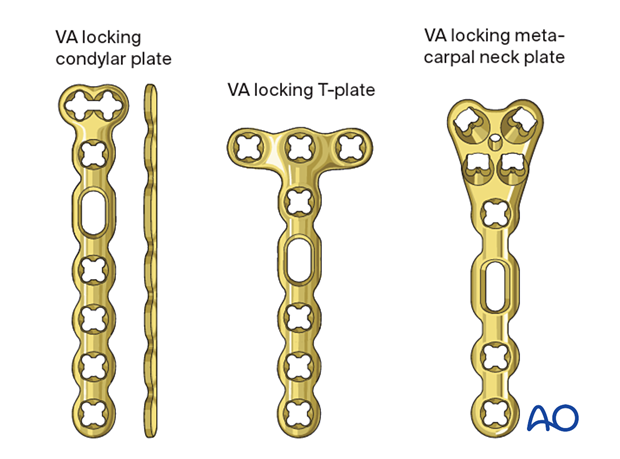
Plate selection
For bridge plating of an extraarticular fracture, several plate types may be used:
- Condylar plate
- T-plate
- Metacarpal neck plate
The plate may need to be contoured to fit the anatomy of the end segment.
The plates come with or without variable-angle (VA) and locking-head screws. For optimal bridging, especially to avoid shortening, locking screws should be used.
The plate selection depends on the fracture pattern and should allow at least two screws in the proximal and distal main fragment.
Usually, 2 mm plates are used for the fixation of the metacarpals. For comminuted fractures, 2.4 mm plates may be indicated.
This procedure shows bridge plate fixation with a condylar plate with VA locking-head screws.
Some plate types have oblong holes, longitudinal and transverse, which allow for correction of axis, length, and rotation after the first two screws are inserted.
AO teaching video
Metacarpal V, neck—Subcapital and comminuted fractures—ORIF using 1.5 mm VA Locking Metacarpal Neck Plate
(6:33)
2. Patient preparation
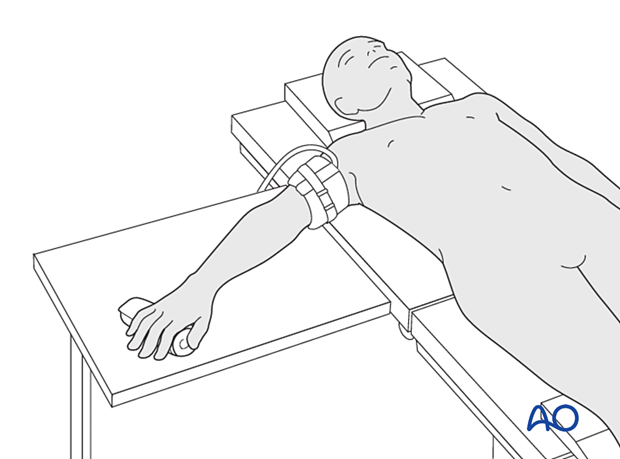
Place the patient supine with the arm on a radiolucent hand table.
3. Approaches
For this procedure, the following approaches may be used:
In the 2nd metacarpal, a radial approach may be used. In the 5th metacarpal, an ulnar approach may be used.
4. Reduction
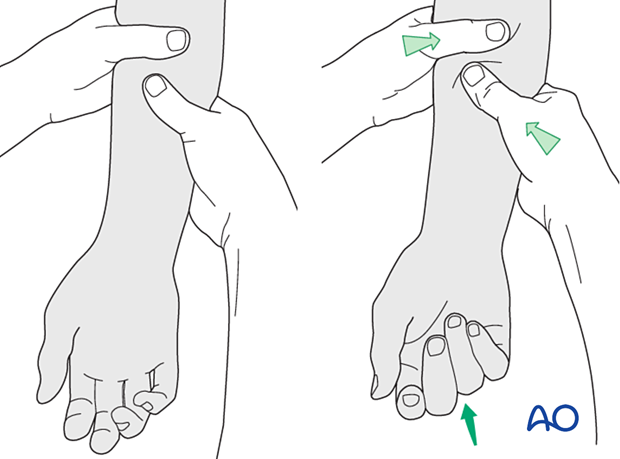
Reduce the fracture preliminarily using longitudinal traction on the finger, manually, using a finger trap, or with pointed reduction forceps.
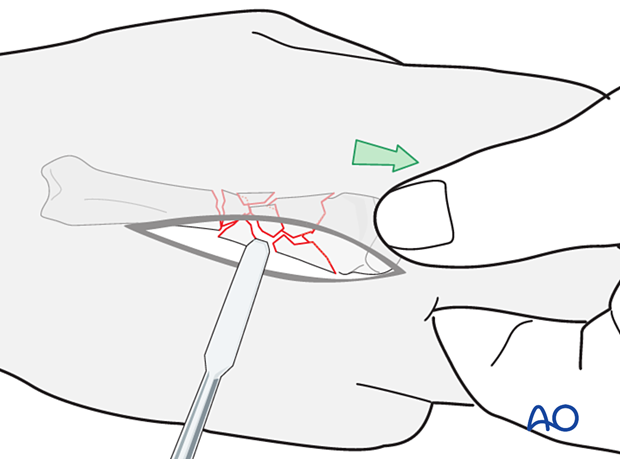
If the periosteum is intact, the small fragments of the comminution are brought into contact with the main fragments when the metacarpal bone is brought out to length.
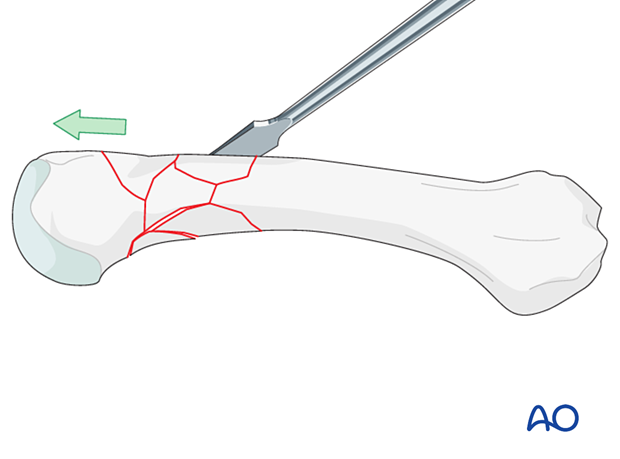
Restoration of length
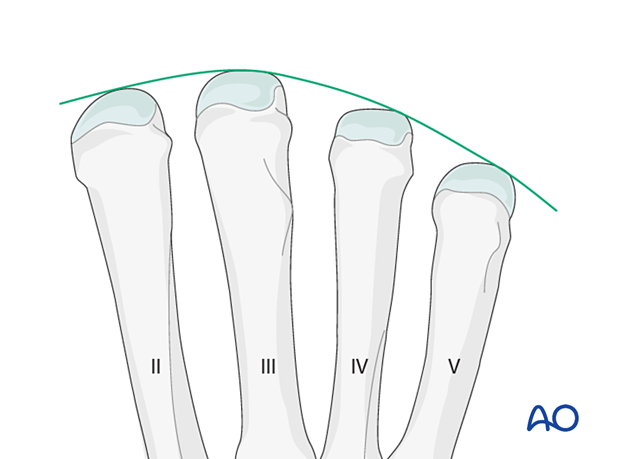
Length should be restored in relation to the neighboring intact metacarpals so that their heads form a gentle arc with its apex over the 3rd metacarpal.
5. Checking alignment
Identifying malrotation
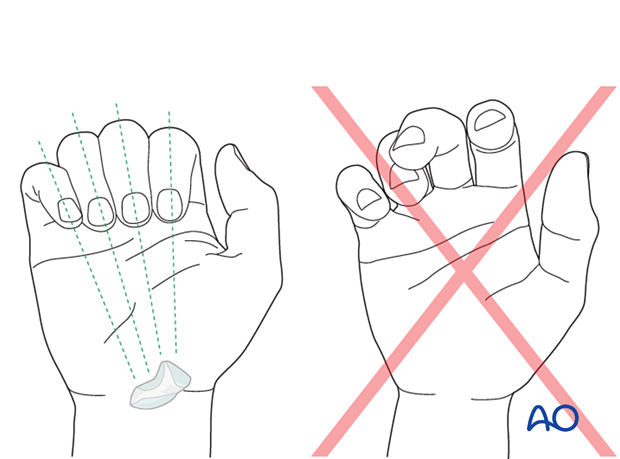
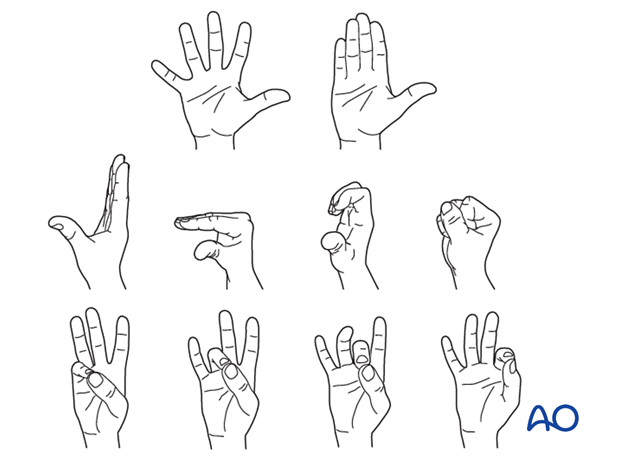
At this stage, it is advisable to check the alignment and rotational correction by moving the finger through a range of motion.
Rotational alignment can only be judged with flexed metacarpophalangeal (MCP) joints. The fingertips should all point to the scaphoid.
Malrotation may manifest by an overlap of the flexed finger over its neighbor. Subtle rotational malalignments can often be judged by a tilt of the leading edge of the fingernail when the fingers are viewed end-on.
If the patient is conscious and the regional anesthesia still allows active movement, the patient can be asked to extend and flex the finger.
Any malrotation is corrected by direct manipulation and later fixed. Flexing the MCP joints while preventing overlap of the fingers will reduce rotational displacement.
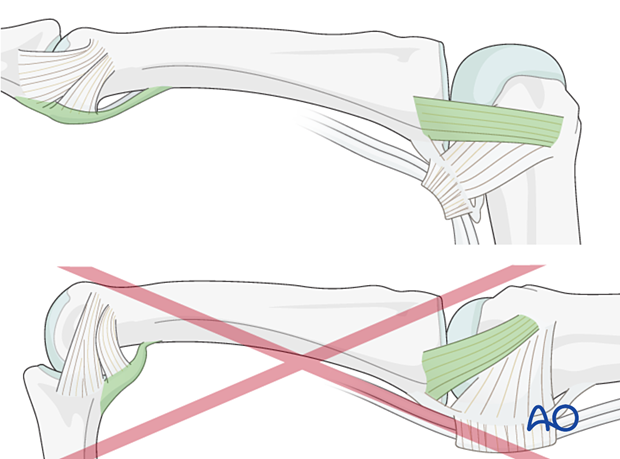
Using the tenodesis effect when under anesthesia
Under general anesthesia, the tenodesis effect is used, with the surgeon fully flexing the wrist to produce extension of the fingers and fully extending the wrist to cause flexion of the fingers.
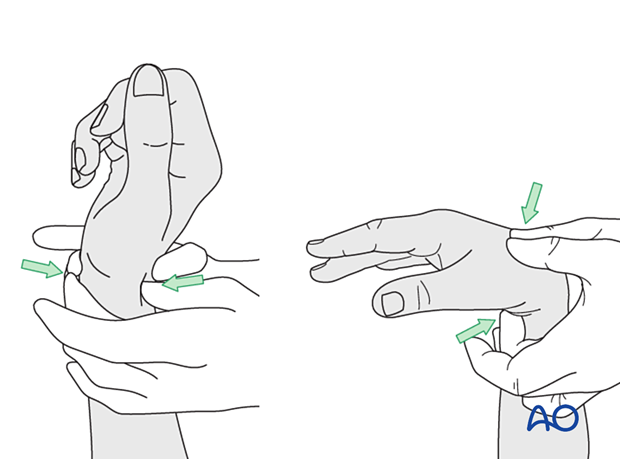
Alternatively, the surgeon can exert pressure against the muscle bellies of the proximal forearm to cause passive flexion of the fingers.
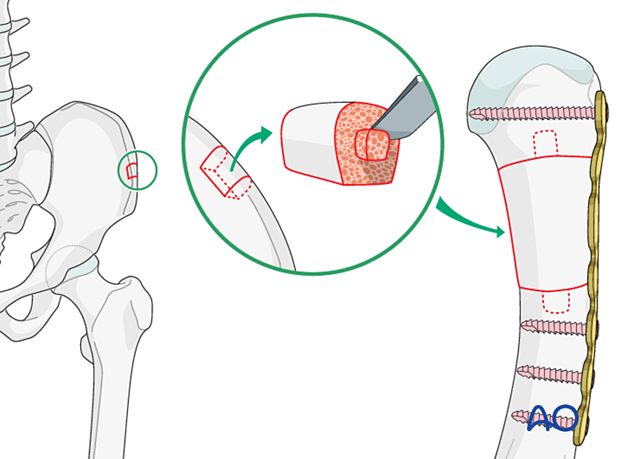
6. Bone grafting
Small bone loss
If there is bone loss but with some bony continuity, the addition of bone graft or substitute is indicated to stabilize the fracture and avoid shortening, especially if a conventional plate with cortical screws has been used.
Severe bone loss
If there is severe soft-tissue compromise and bone loss (no bony continuity), the addition of a tricortical bone graft harvested from the iliac crest or distal radius may be used.
The graft may be shaped with a spike on both ends to fit into the intramedullary cavity of the main fragments. This provides intrinsic stability to the graft.
7. Plate preparation
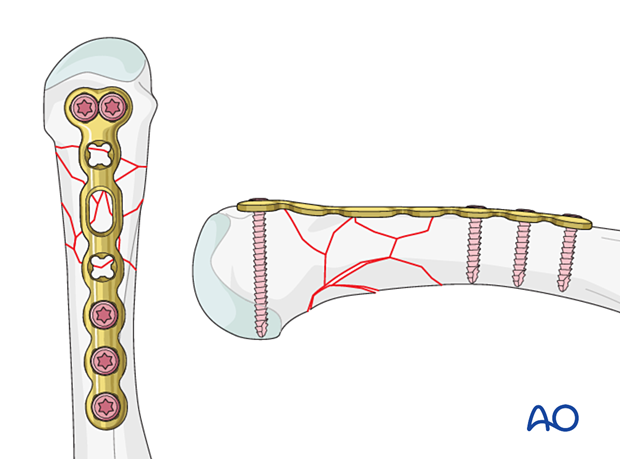
Plate position
The plate position is usually dorsally onto the metacarpal in its long axis. In the 2nd and 5th metacarpal, the plate may be placed radially and ulnarly, respectively.
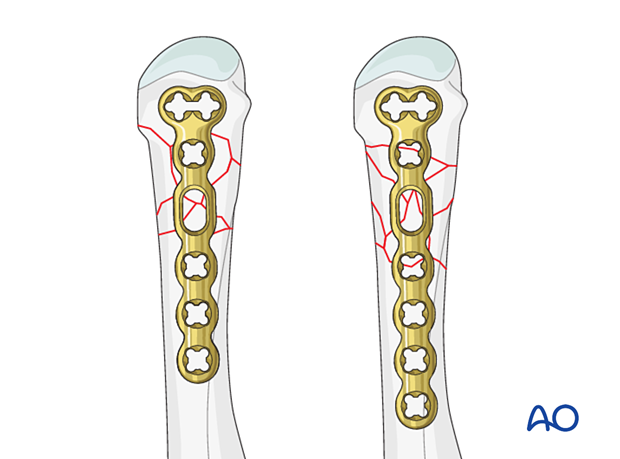
Plate trimming
Adapt the plate length to the length of the metacarpal. Avoid sharp edges, which may be injurious to the tendons. There should be at least 3 plate holes proximal to the fracture available for fixation in the diaphysis. At least two screws need to be inserted into the diaphysis.
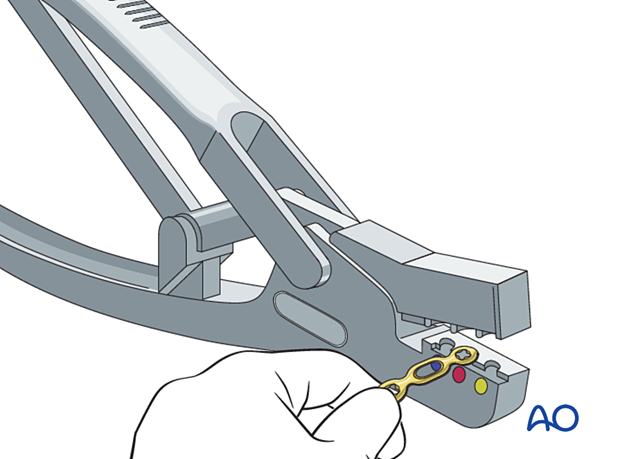
Contouring
Contour the plate to conform with the normal shape of the metacarpal.
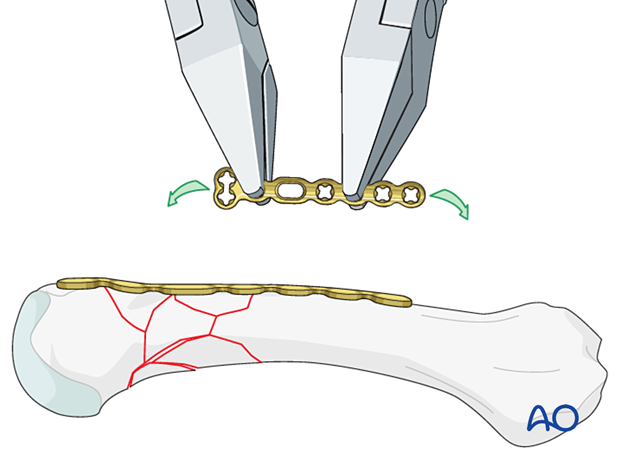
Check for perfect adaptation of the plate to the end segment of the metacarpal.
If it is not perfectly adapted, fracture displacement or malrotation may occur.
8. Plate fixation
Plate application
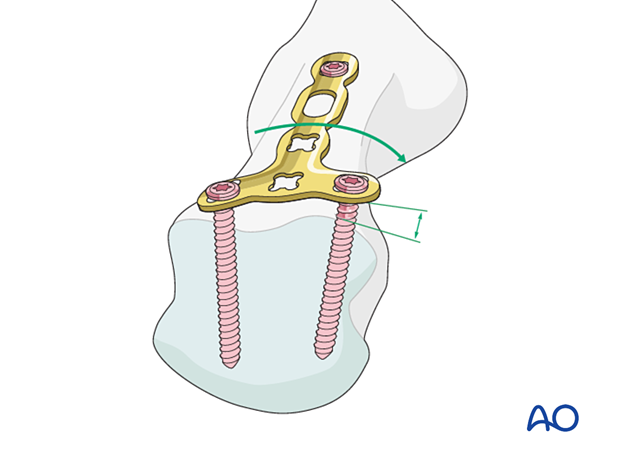
Place the plate dorsally on the bone, as distally as possible, without interfering with the joint. The distal end of the plate should be slightly proximal to the articular surface of the head.
Ensure that the plate is centered on the diaphysis in the coronal plane.
Keep the plate in place with the atraumatic forceps.
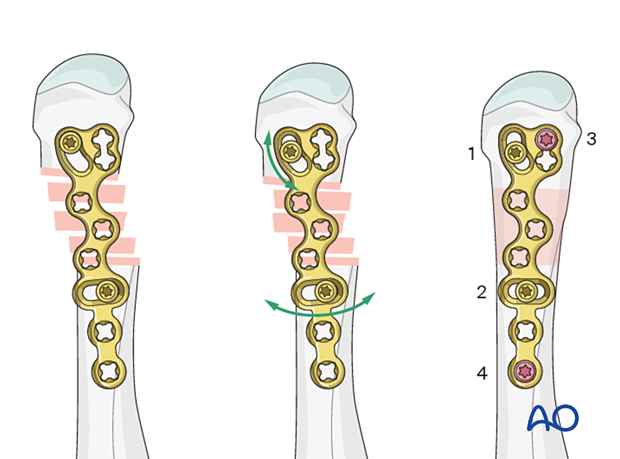
Screw insertion (distal)
Start with inserting two screws into the articular block:
Carefully drill the first screw hole through the transverse plate part with a 1.5 mm drill bit. The drill bit should engage but not penetrate the far cortex.
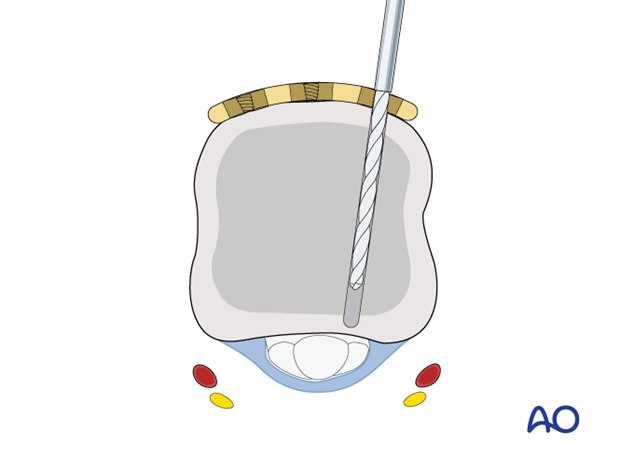
Insert the first screw. Ensure that it engages the far cortex but does not protrude into the fibro-osseous flexor digital channel, where the flexor tendons run. The digital nerve and artery are also at risk of injury.
Insert a second screw into the opposite end of the transverse plate section in the same fashion, alternately tightening both screws.
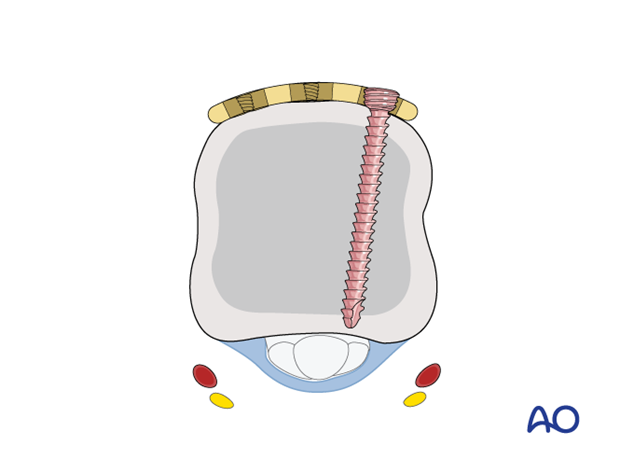
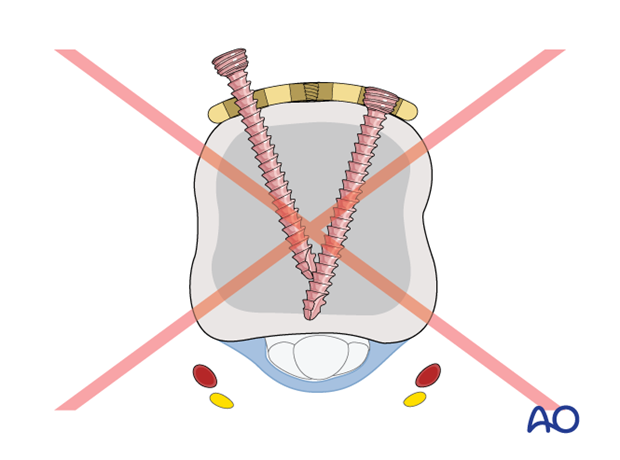
Pitfall: interfering screws
Checking alignment
Confirm correct axial alignment and length with an image intensifier. Check correct rotation by flexing all fingers at the metacarpophalangeal (MCP) joints.
Correct rotational alignment of the distal main fragment may be difficult to achieve but is essential.
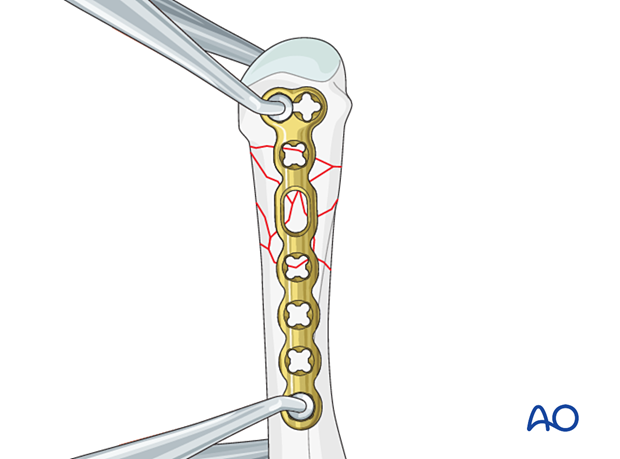
Screw insertion in the other main fragment
Ensure the plate is correctly aligned in the longitudinal axis of the metacarpal. Insert a screw into the other main fragment in the same fashion as above.
Some plates allow for correction of axis, length, and rotation after the first two screws are inserted.
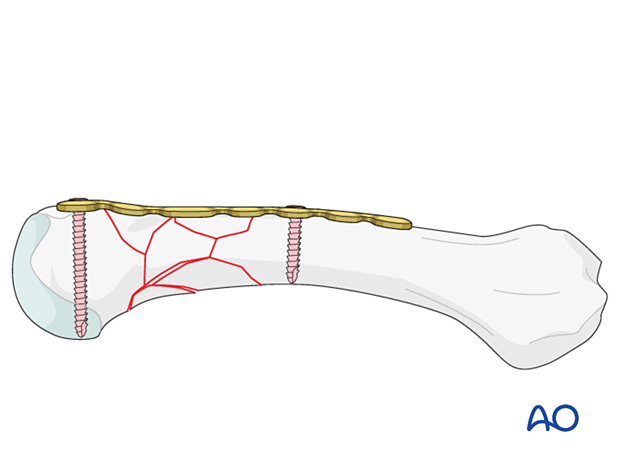
Finalizing fixation
Insert further screws in the same fashion so that at least two screws are in both main fragments.
Cover the plate with periosteum to avoid adhesion between the tendon and the implant leading to limited finger movement.
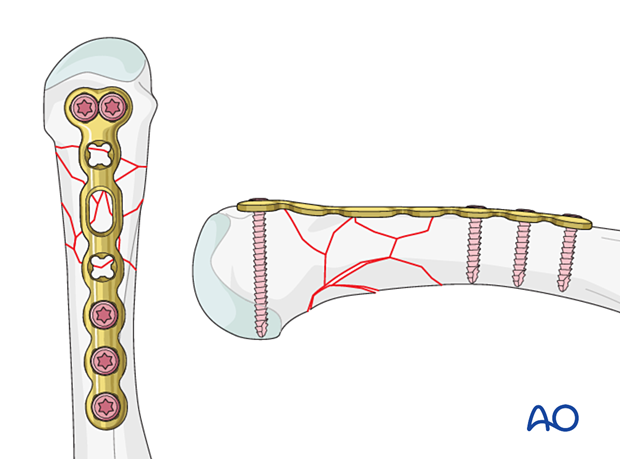
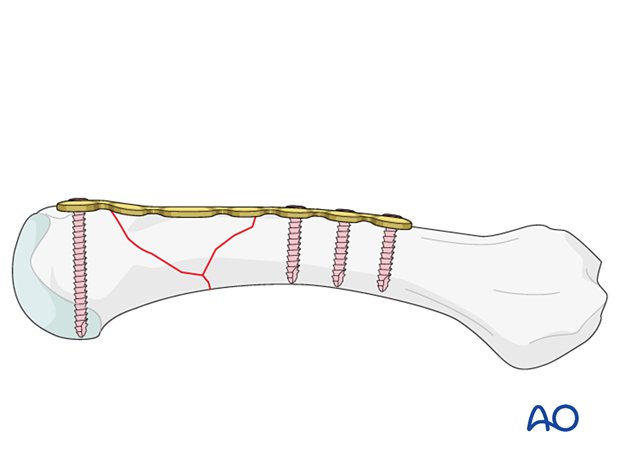
Final bridging construct of a wedge fracture
9. Final assessment
Clinically confirm correct rotational alignment again.
Confirm reduction and correct placement of implants in AP, lateral, and oblique views.
10. Aftercare
Postoperative phases
The aftercare can be divided into four phases of healing:
- Inflammatory phase (week 1–3)
- Early repair phase (week 4–6)
- Late repair and early tissue remodeling phase (week 7–12)
- Remodeling and reintegration phase (week 13 onwards)
Full details on each phase can be found here.
Postoperative treatment
If there is swelling, the hand is supported with a dorsal splint for a week. This would allow for finger movement and help with pain and edema control. The arm should be actively elevated to help reduce the swelling.
The hand should be splinted in an intrinsic plus (Edinburgh) position:
- Neutral wrist position or up to 15° extension
- Metacarpophalangeal (MCP) joint in 90° flexion
- Proximal interphalangeal (PIP) joint in extension
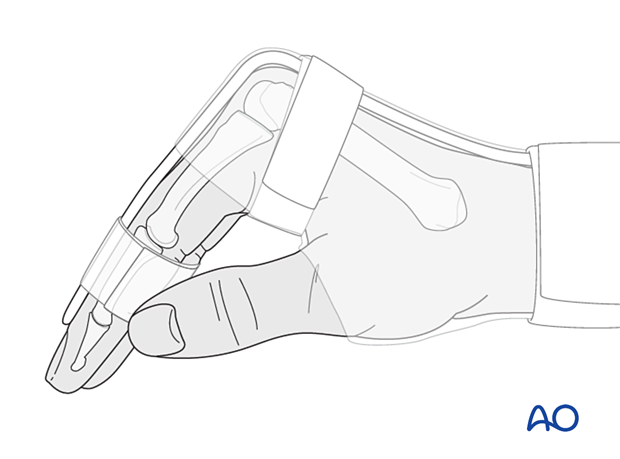
The reason for splinting the MCP joint in flexion is to maintain its collateral ligament at maximal length, avoiding scar contraction.
PIP joint extension in this position also maintains the length of the volar plate.
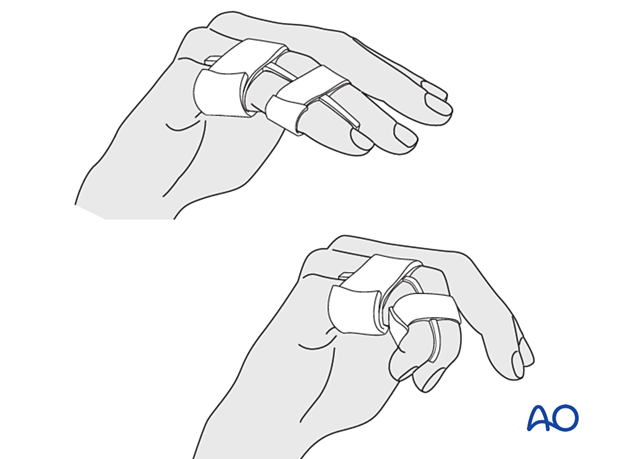
After subsided swelling, protect the digit with buddy strapping to a neighboring finger to neutralize lateral forces on the finger.
Functional exercises
To prevent joint stiffness, the patient should be instructed to begin active motion (flexion and extension) immediately after surgery.
Follow-up
See the patient after 5 and 10 days of surgery.
Implant removal
The implants may need to be removed in cases of soft-tissue irritation.
In case of joint stiffness or tendon adhesion restricting finger movement, arthrolysis or tenolysis may become necessary. In these circumstances, the implants can be removed at the same time.












