Assessment of elbow stability
1. Identification of elbow subluxation or dislocation
Generally, elbow subluxation and dislocation are discovered on radiographs taken for pain, deformity, swelling and ecchymosis, or crepitation.
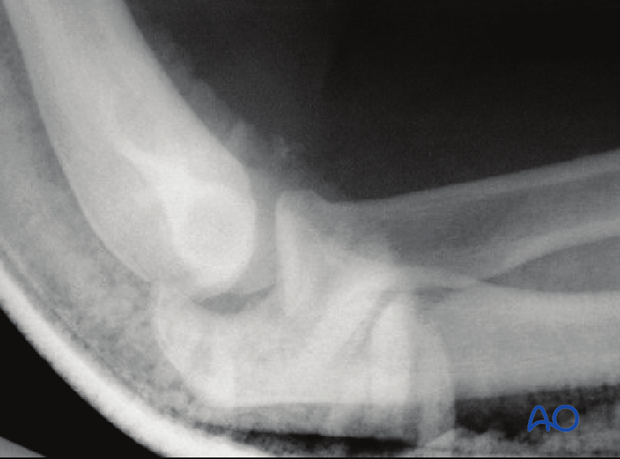
2. Subtle radiographic signs of subluxation
Subluxation can be subtle.
On a posteroanterior radiograph either the medial ulnotrochlear or the radiocapitellar articulation may be gapped more than expected.
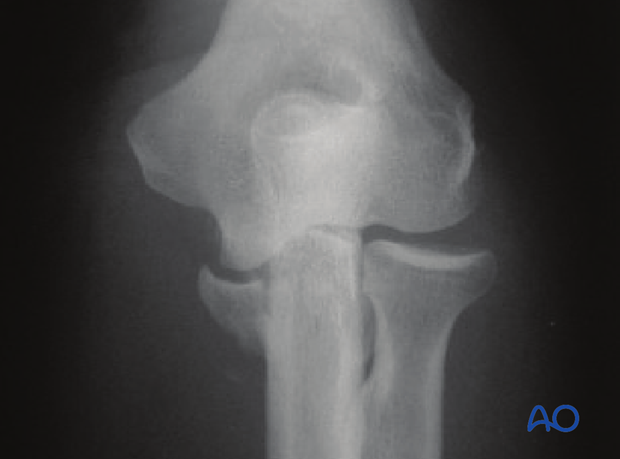
On a lateral radiograph, a line bisecting the radial shaft may not pass through the middle of the capitellum, and there may also be a slight gap or “drop sign” in the ulnohumeral joint.
3. After reduction: physical examination for dislocation
The medial and lateral epicondyles and the tip of the olecranon should all lie in a single plane parallel to the shaft of the humerus.
If the tip of the olecranon seems anterior to the plane, the elbow is likely dislocated.
4. After reduction: check stability
For simple elbow dislocations, if the patient is awake enough to participate after reduction, one can ask the patient to move the elbow through an arc of flexion and extension to see if the elbow re-dislocates.
This should not be done for fracture-dislocations as they are expected to be less stable.
Since most elbow dislocations result in complete or near complete capsuloligamentous disruption, varus and valgus instability are expected and do not need to be tested.
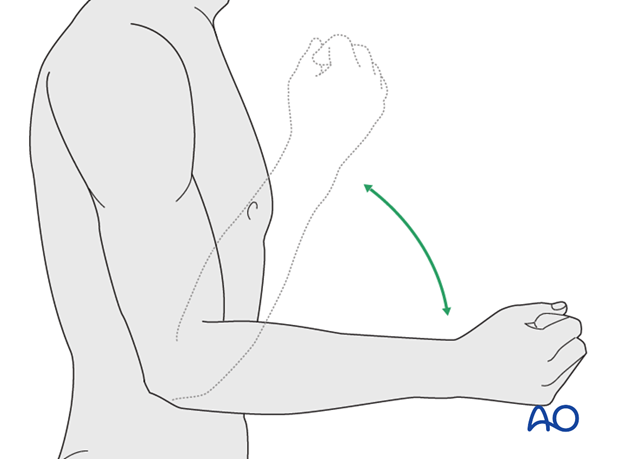
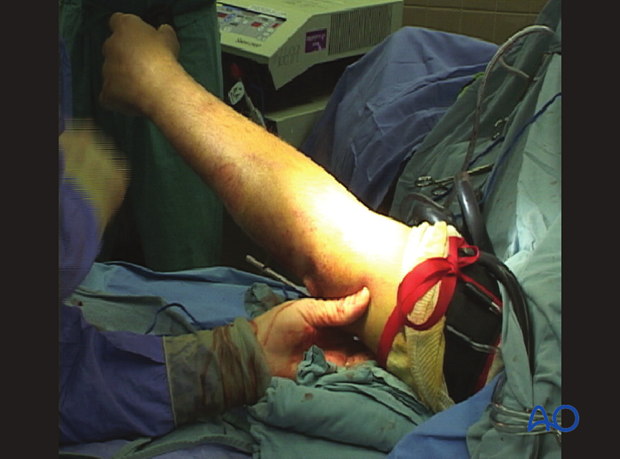
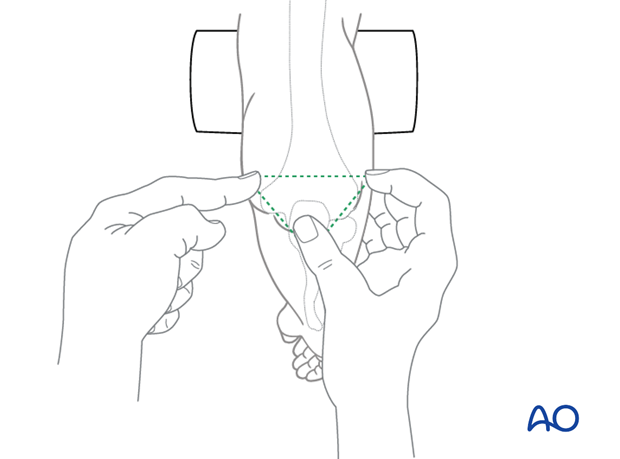
5. After surgery: check stability
After surgery to stabilize the elbow, place the elbow in full gravity extension with the forearm in neutral to see if it subluxates (check under image) or dislocates (feel for a clunk as it is relocated). There is no need to test an unrepaired medical collateral ligament as we expect it to be valgus unstable.