Complications and technical failures
1. Introduction
Femoral fractures are often high-energy injuries and are associated with significant but predictable complications including limb-threatening vascular injuries.
Growth-plate injury is common following distal femoral fractures and early diagnosis is important to avoid progressive malalignment.
2. Vascular injuries
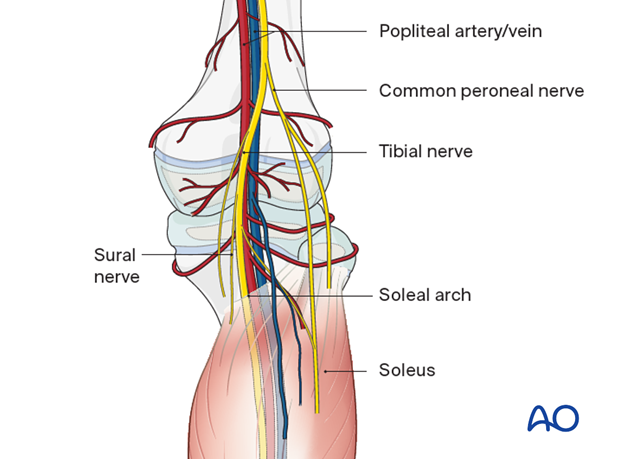
The popliteal vessels are at risk of injury with distal femoral and proximal tibial fractures.
This is particularly relevant in the presence of significant displacement because the neurovascular bundle is fixed at the soleal arch.
Arterial injuries include transection, major branch avulsion and intimal tears. Limb ischemia may occur immediately following injury or develop in the subsequent hours or days.
Compartment syndrome can develop after partial or temporary ischemia.
Diagnosis:
- High index of suspicion with displaced fractures
- Record foot pulses, skin color and temperature
- Examine distal muscle groups for stretch pain and worsening pain out of proportion with the injury
- Measure ankle brachial index
- Consider doppler ultrasound, angiogram, or CT angiogram but do not delay reduction of fracture
Treatment:
- Urgent fracture reduction and stabilization
- Collaborate with a surgeon capable of vessel exploration and repair
- Consider prepping the contralateral limb for vein graft
- Consider prophylactic fasciotomy if the ischemic time exceeds 6 hours
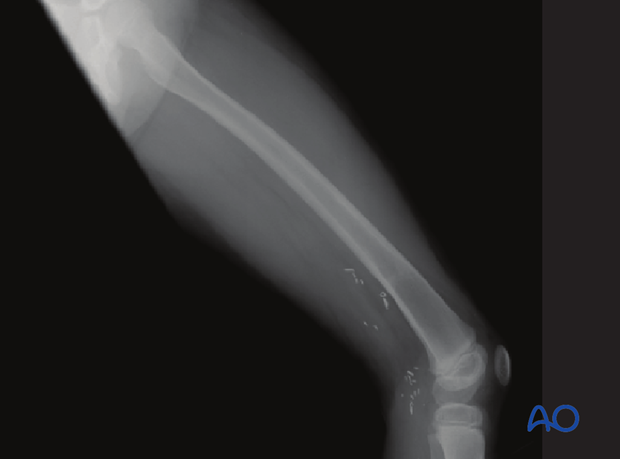
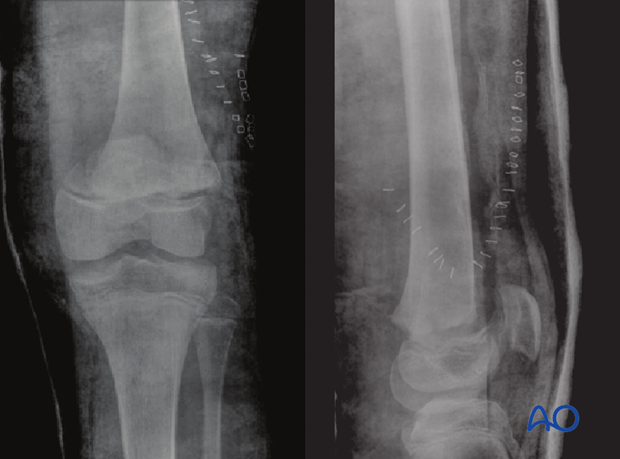
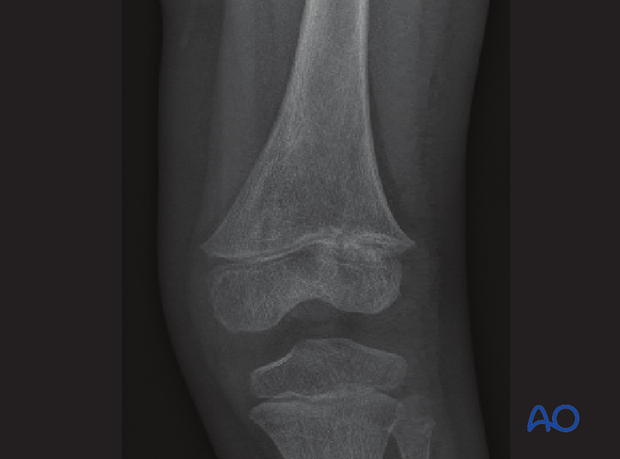
The x-ray shows significant anterior displacement and shortening of a Salter-Harris II fracture in a 6-year-old female. The patient had a pulseless white foot and a complete transection of the popliteal vessels.
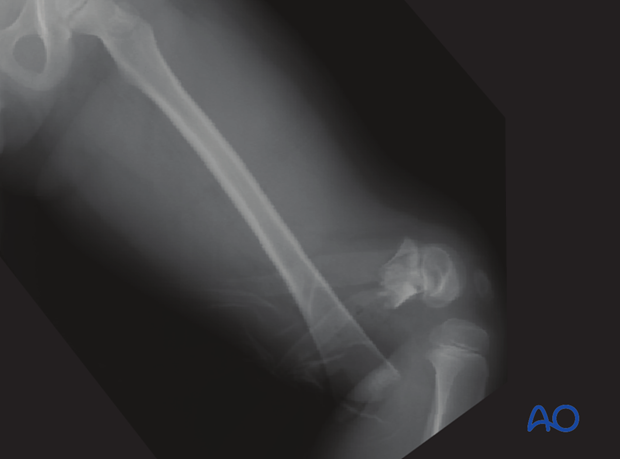
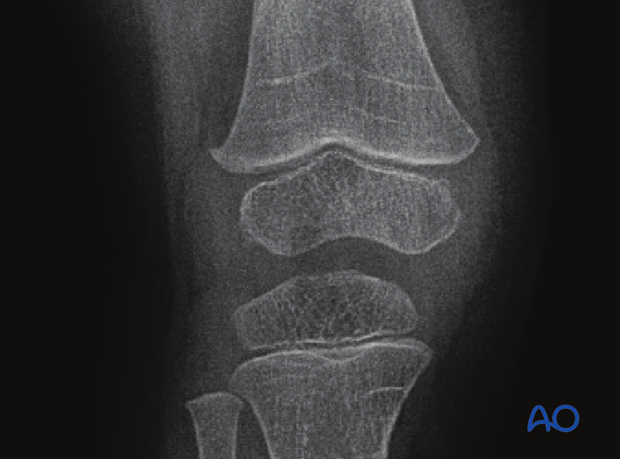
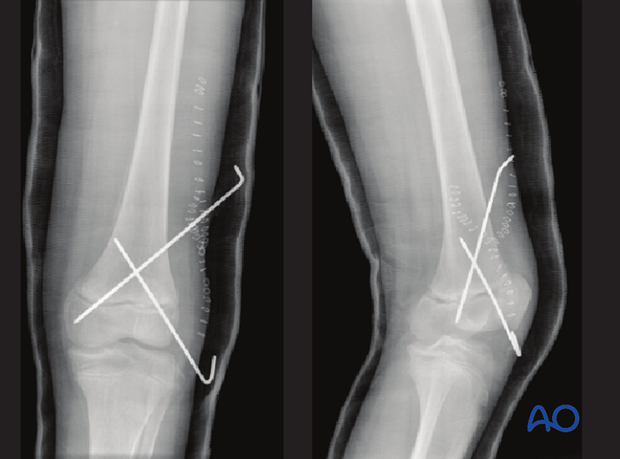
X-ray of the healed fracture after removal of K-wires. Vascular clips show the location of the open vessel repair.
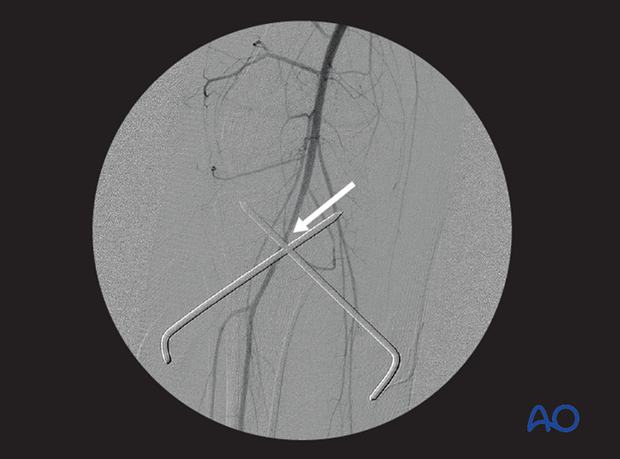
Angiogram following proximal tibial growth plate injury shows partial occlusion of the popliteal artery. The narrowed vessel on the angiogram corresponds to tearing of the vessel intima.
Clotting resulted in complete occlusion of the vessel two days later.
3. Growth-plate injuries
Injury to the growth plate is common after all patterns of distal femoral fracture.
All patients should be followed to demonstrate that growth has resumed or to ensure early diagnosis of growth-plate injury.
Recommended reading:
- Nguyen JC, Markhardt BK, Merrow AC, et al. Imaging of Pediatric Growth Plate Disturbances. Radiographics. 2017 Oct;37(6):1791–1812.
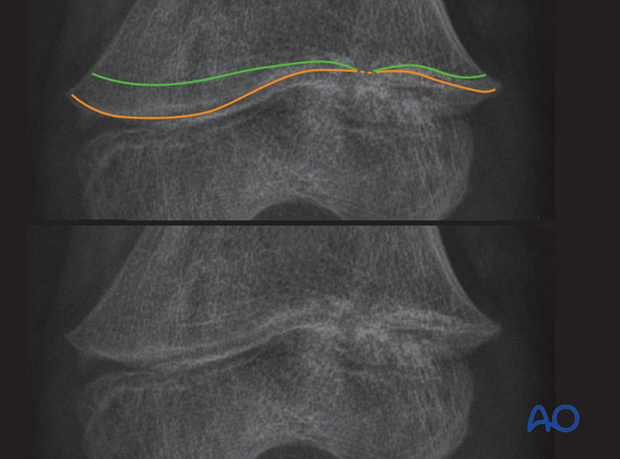
In this case the x-ray shows complete Harris lines in the metaphysis.
They are parallel to the growth plate indicating normal growth.
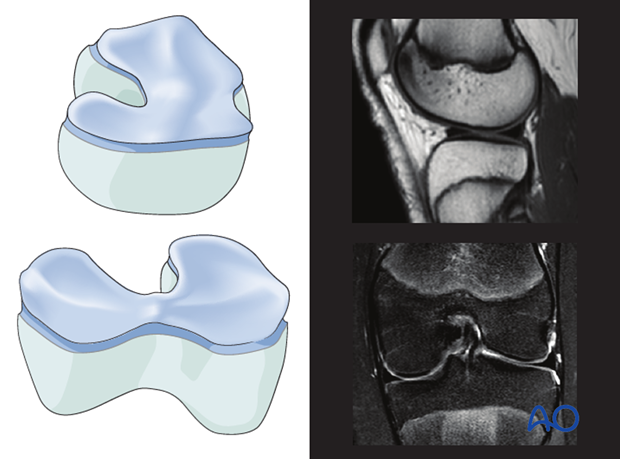
Anatomy of distal femoral growth plate
The growth plate of the distal femur has multiple undulations in both coronal and sagittal planes. The epiphysis and metaphysis interdigitate and this resists shearing forces.
Clinical consequences:
- Higher energy to cause growth-plate disruption
- Fracture may cross all zones of the growth plate
- Growth plate injury occurs in up to 50% of patients
Complete closure of distal growth plate
A fracture pattern with a large transverse disruption of the growth plate is more likely to cause a uniform growth arrest.
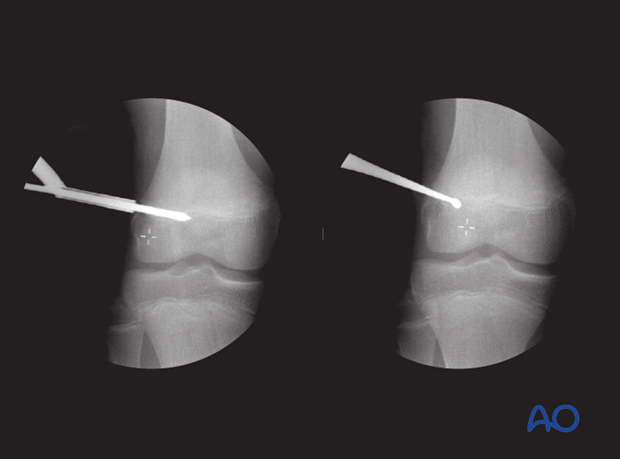
In this case a partial reduction of a Salter-Harris II fracture with a small medial metaphyseal fragment is seen.
Anatomic reduction of the fracture has been performed and smooth K-wires used for stabilization to minimize secondary damage to the growth plate.
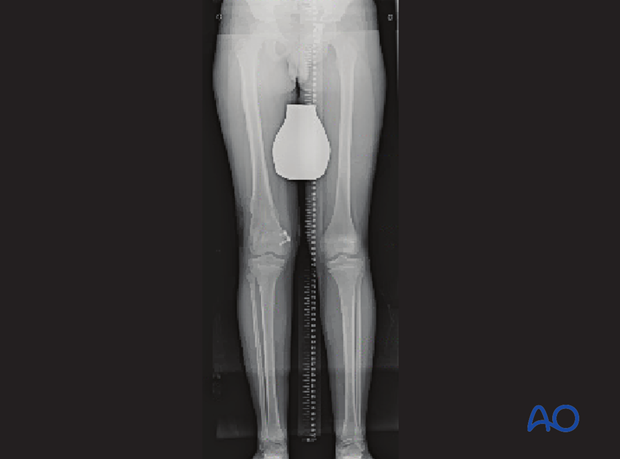
At 12 weeks the affected left distal femoral physis is completely closed. The contralateral side has a wide-open growth plate.
Note the horizontal sclerotic Harris line showing proximal tibial growth on the left side since the fracture.
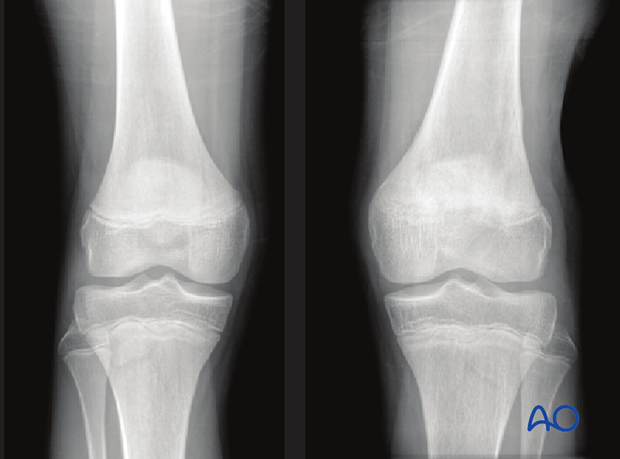
Options for ensuring leg length equality at maturity include epiphysiodesis of the opposite side (illustrated) or surgical lengthening of the affected leg.
Partial closure of distal growth plate
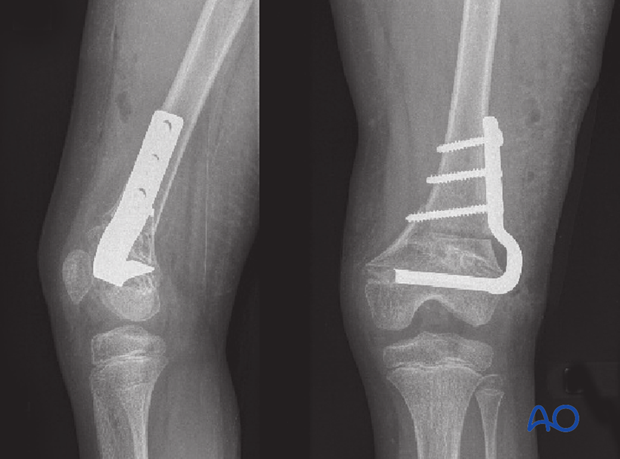
Case 1This 9-year-old boy was a pedestrian struck by a motor vehicle. He sustained a displaced Salter-Harris II fracture of the distal femur.
The lateral growth plate is completely disrupted but the medial growth plate is protected by the large metaphyseal (Thurstan Holland) fragment.
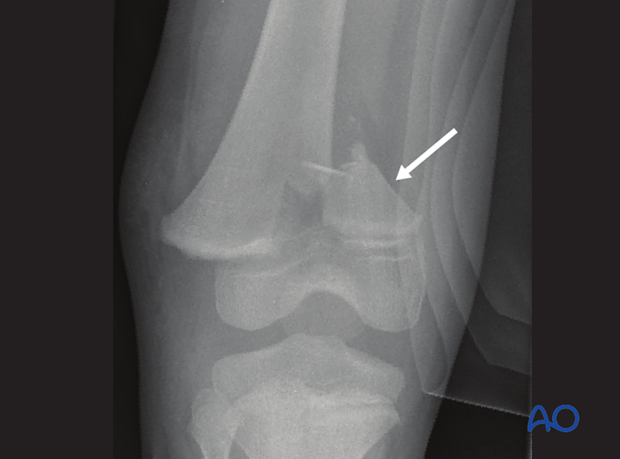
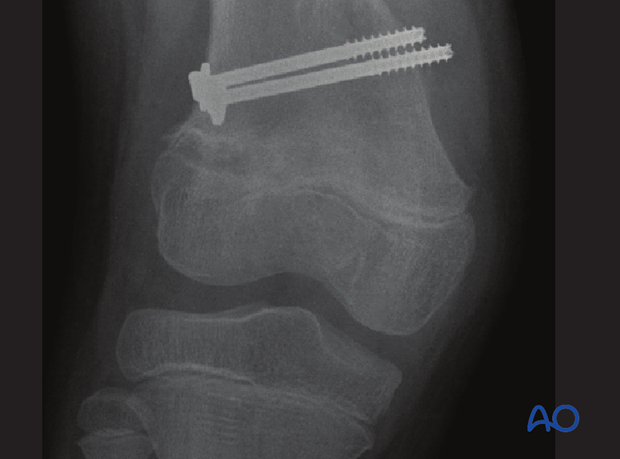
The fracture has been stabilized with metaphyseal cannulated screws and protected in a cast.
The patient is at high risk of partial or complete growth plate closure and should be followed closely until growth is proven to resume.

He missed two years of follow-up.
There is significant valgus deformity due to ongoing growth of the medial side of the growth plate but cessation on the lateral side.
Earlier diagnosis would mean less deformity and more straightforward treatment.
Standing x-ray shows significant shortening and deformity.
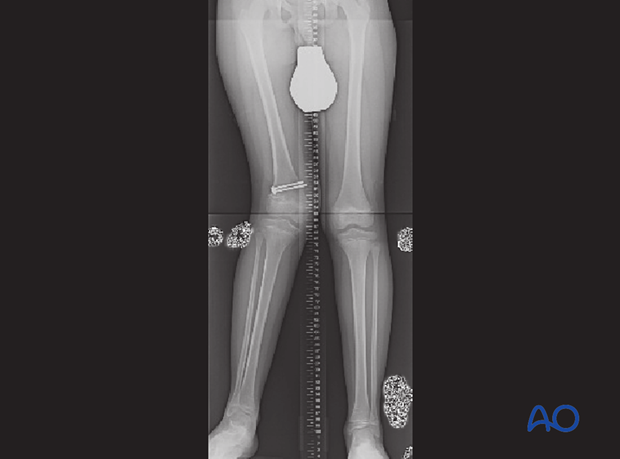
Treatment included gradual deformity correction with leg lengthening and completion of epiphysiodesis on the medial side.
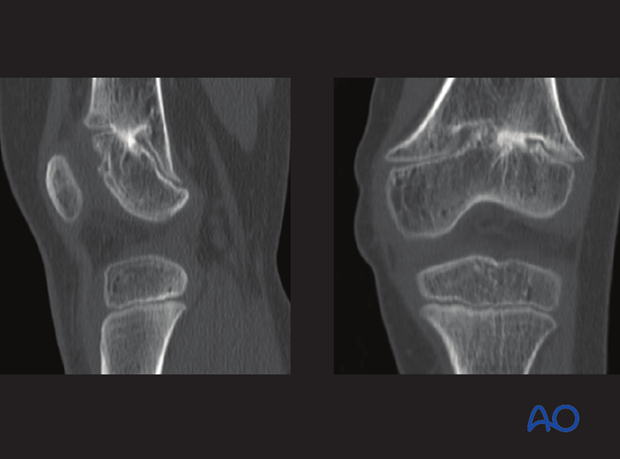
This 5-year-old female has incomplete reduction of a Salter-Harris II fracture stabilized with K-wires. The gap visible centrally in the physis may permit bony ingrowth and bar formation.
Immediate postoperative films also demonstrate varus angulation.
The medial side of the growth plate has its metaphyseal portion attached and is relatively protected.

At 12 weeks the irregularity in the lateral half of the growth plate suggests early bony bar formation.
Closer inspection shows growth lines converging toward the site of the early bar. But the finding at this time is subtle and the diagnosis was not made.
MRI imaging allows the growth plate to be directly visualized and demonstrates a physeal bar.
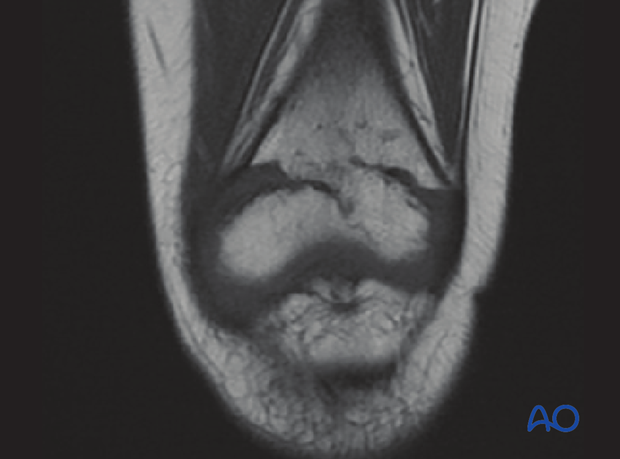
Later CT imaging confirms an anterolateral bony bar which has produced a valgus and substantial extension deformity.
Clinically the knee hyperextended by 30° and the valgus deformity was evident.

Osteotomy was used to correct the deformity. Length inequality will be addressed in a later procedure.
Earlier diagnosis of the bar may have resulted in less deformity and simplified treatment eg, bar excision or completion of epiphysiodesis.
Anatomic reduction may have prevented formation of this bar. However, some bars will form even after anatomic reduction due to the injury to the germinal layer.
4. Angular deformity following incomplete reduction
Experimental physeal disruption
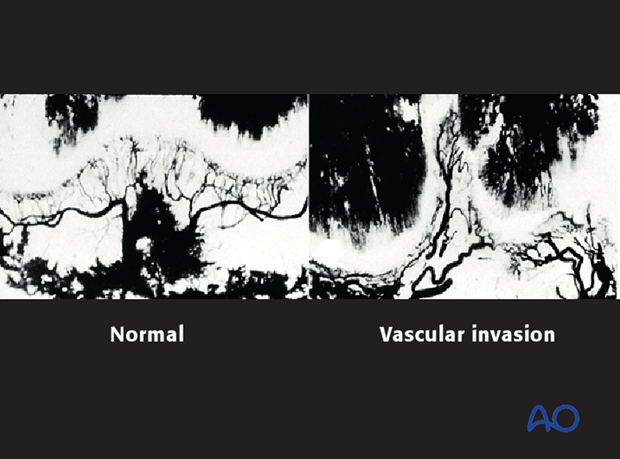
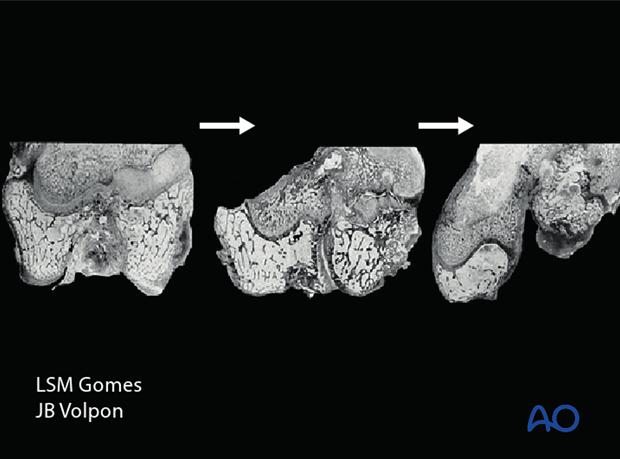
Gomes and Volpon investigated the evolution of physeal bars after Salter-Harris IV injuries, at a histological level.
- Gomes LSM, Volpon JB. Experimental physeal fracture-separations treated with rigid internal fixation. J Bone Joint Surg Am. 1993 Dec;75(12):1756–1764.
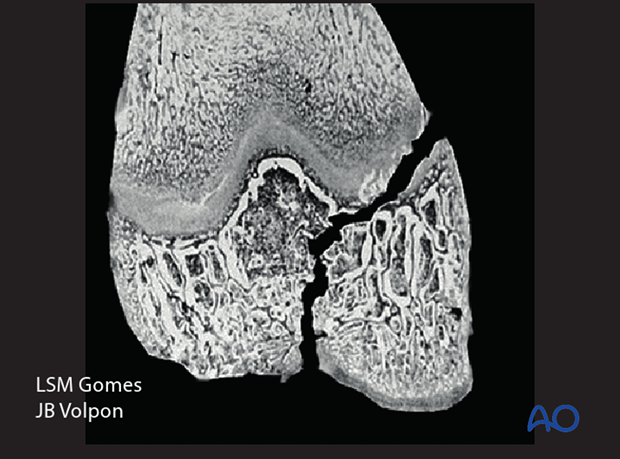
They demonstrated that if the transphyseal fracture plane was not surgically closed and stabilized, vessels invaded the fracture plane, forming a bony tether across the physis. This led to a locus of growth arrest.
Clinical implication: Anatomical reduction of physeal injuries should reduce the risk of growth arrest.