Direct lateral approach to the proximal femur
1. Preliminary remarks
Scar tissue due to previous exposure might obscure typical landmarks.
The direct lateral approach releases the anterior third of gluteus medius and minimus, while preserving the posterior femoral attachment of the major part of these muscles. The proximal part of the incision is limited by the superior gluteal nerve and vessels, crossing 3-5 cm proximal to the tip of the greater trochanter. Distally, the anterior fibers of vastus lateralis are elevated from the anterior femur. The anterior attachment of the hip capsule is next released from the anterior base of the femoral neck, and an anterior longitudinal capsulotomy is opened as necessary with a proximal transverse “T”.
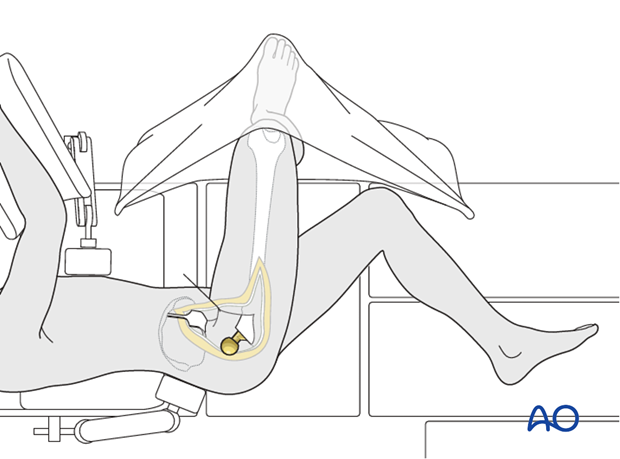
This approach can be done with the patient in lateral decubitus position or supine. It is excellent for periprosthetic fractures of the proximal femur and could be used for revision arthroplasty.
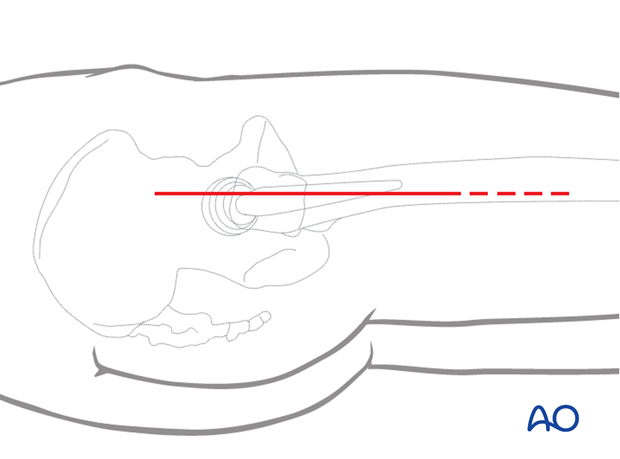
2. Skin incision
Make a longitudinal incision through skin and subcutaneous tissue.
Carry it down to the fascia lata.
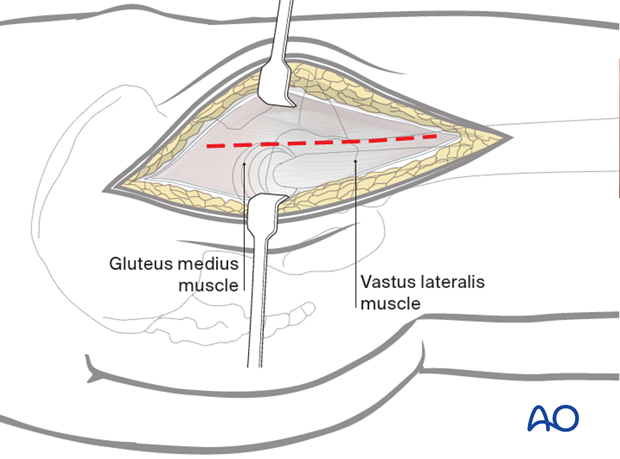
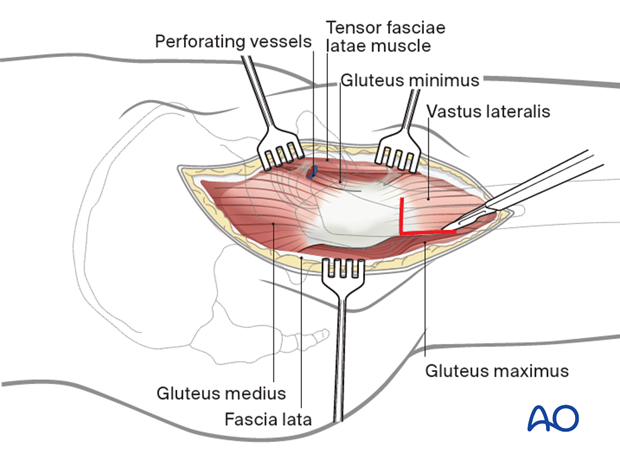
3. Superficial surgical dissection
Divide the fascia lata over the greater trochanter, extending it distally over the proximal femoral shaft at the anterior border of gluteus maximus to reveal the underlying gluteus medius.
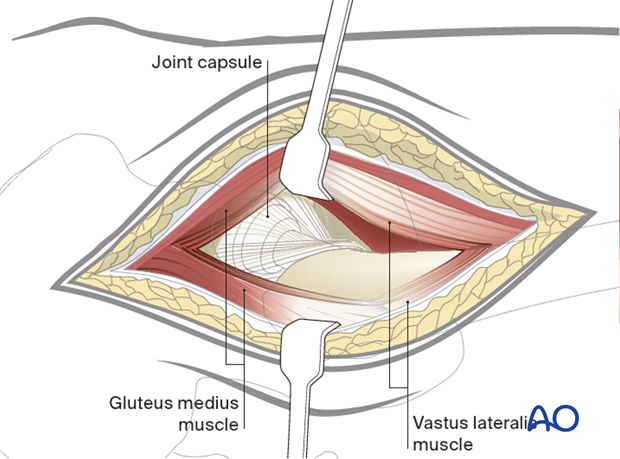
4. Deep surgical dissection
Remove bursal tissue over the trochanter as needed.
Outline an incision to release the anterior gluteus medius from the greater trochanter. Proximally, this extends into the tendinous insertion of gluteus medius proximally and splitting fibers of vastus lateralis distally. Preserve a substantial portion of gluteus medius insertion posteriorly.
The exposure can be extended distally through a subvastus approach.
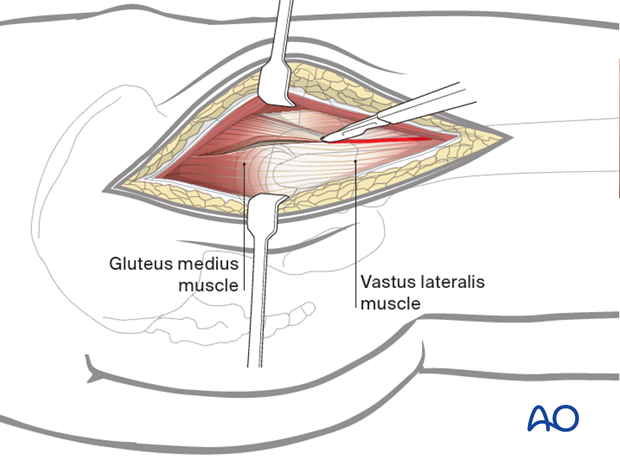
Deepen the incision through the gluteus medius and minimus proximally, retracting the anterior flap to show the hip capsule superiorly and adjacent supraacetabular ilium. Extend the incision distally, along the anterolateral femoral shaft and then release the intervening tissue from the anterior intertrochanteric region, sharply releasing the hip capsule from the anterior femur.
Release the capsule sufficiently anteroinferiorly and anterosuperiorly to expose the prosthesis and permit free external rotation of the femur. Make a T– shaped capsulotomy to expose the prosthesis.
The vastus lateralis can be released from its origin to further expose the proximal femur.
Exposure of the proximal femur and prosthesis is gained by gentle external rotation of the leg. The hip may be dislocated if necessary. The lower leg is placed into a pocket made from sterile drapes.
Use retractors as necessary to expose the prosthesis.
For revision hip arthroplasty, retraction of the proximal femur distally will allow exposure of the acetabular component.
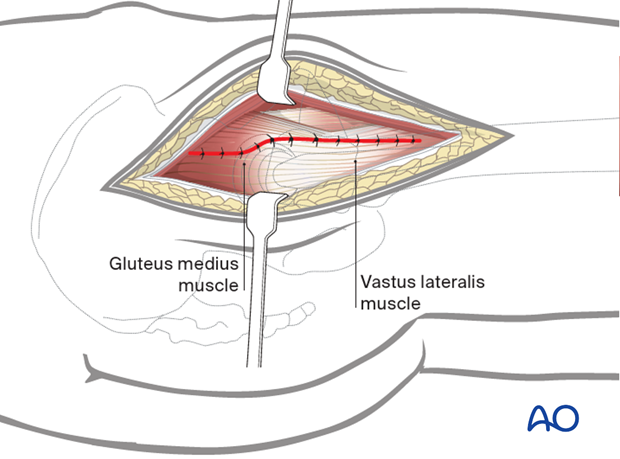
5. Wound closure
Heavy sutures, typically placed through holes in the bone, are used to reattach the anterior flap to the intertrochanteric region. Also close the gluteus medius tendon and fascia proximally, and the vastus lateralis fascia distally.
Repair the vastus lateralis to its origin.
Close the fascia lata, subcutaneous tissue and skin as desired.
Considerations for periprosthetic fracture patients
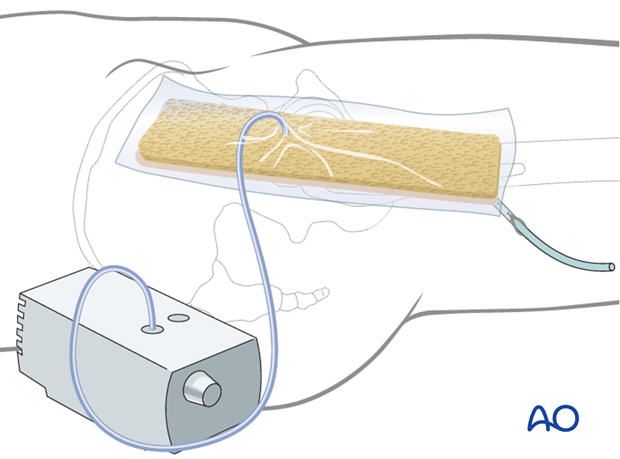
A layered closure is preferred for periprosthetic fractures. A subfascial drain should be considered as blood loss can be significant and periprosthetic fracture patients are at high risk of requiring anticoagulation immediately postoperatively. A hematoma requiring evacuation must be avoided. The wound is closed in layered fashion according to the surgeon's preference.
Sterile dressing should be applied, and negative pressure incisional wound care can be considered.