Patient examination
1. General considerations
Age
Usually older age is associated with a lower chance of curve progression while patients presenting with the same degree of curve at a younger age has a higher chance of curve progression that may reach surgical indications.
Curve magnitude at presentation
Curves less than 20° at presentation can usually be followed while those presenting between 20° and 30° will usually undergo a trial of brace treatment. If a patient presents with a curve magnitude greater than 40° the chances of needing surgery eventually is high.
Length of time post menarche
Length of time post menarche is an indication of skeletal maturity. A person grows fastest one year before onset of menarche and usually finishes growing two years after its onset.
Presence of positive patient family history
AIS is an inherited condition with familial associations. A careful family history should always be taken.
2. Physical examination
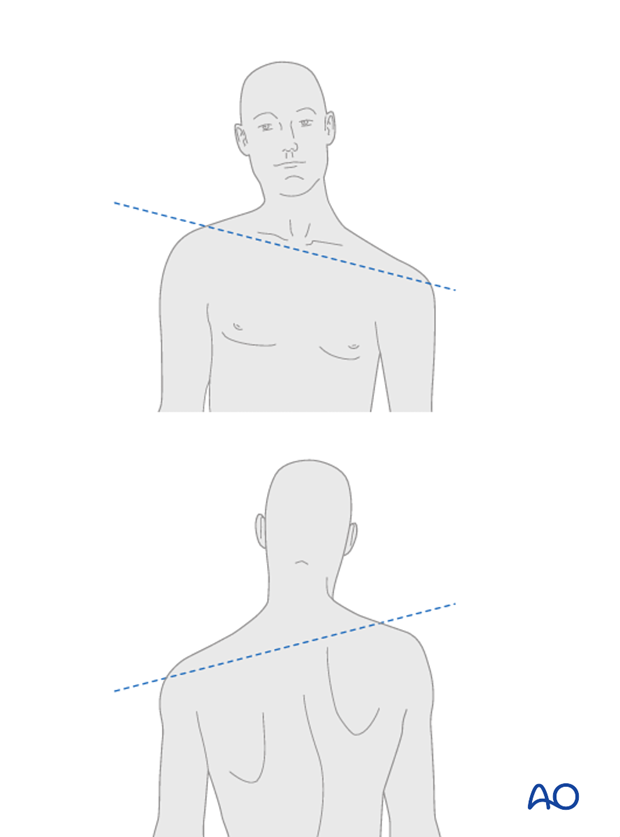
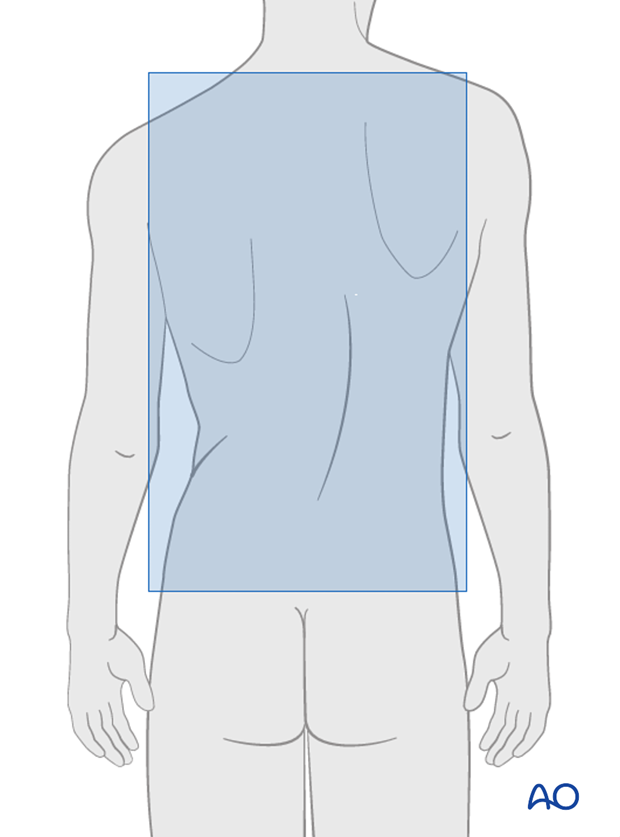
Assessment of shoulder balance
Shoulder balance can be assessed looking at the patient posteriorly as well as anteriorly. If one shoulder is higher than the other it should be noted.
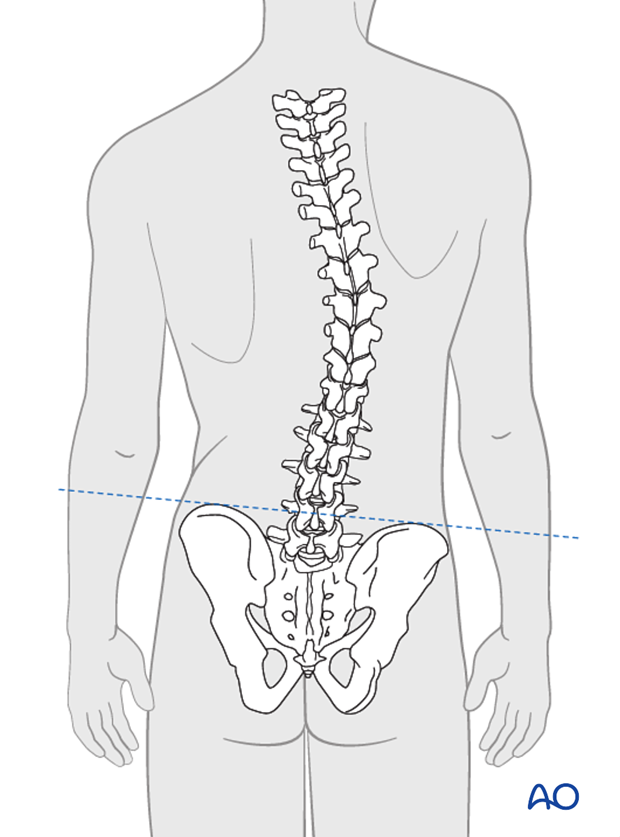
Assessment of waist crease/pelvic obliquity
Presence of asymmetry of waist crease, truncal shift and pelvic obliquity should also be assessed by direct visualization.
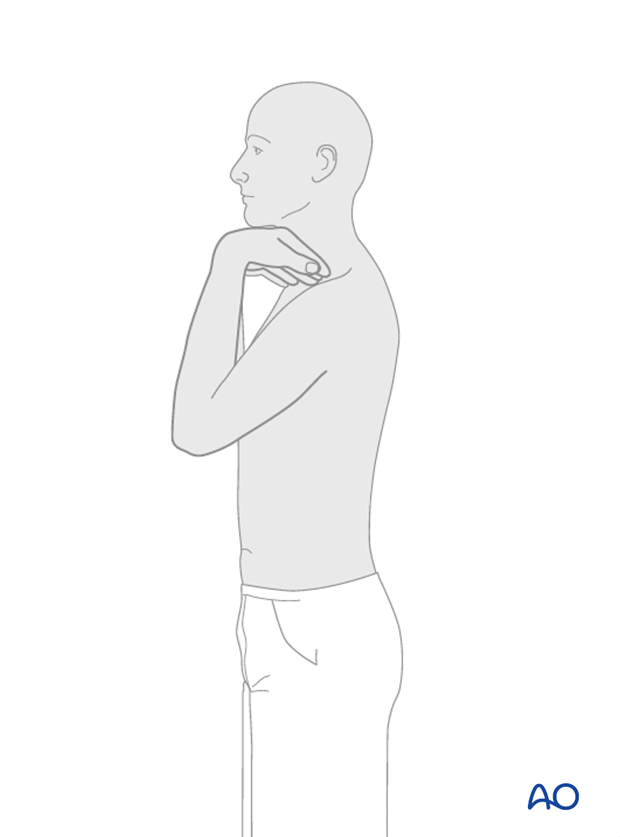
Assessment of angle of trunk rotation
A scoliometer is used to assess angle of trunk rotation for the thoracic as well as the lumbar prominence while the patient is a forward bending position.

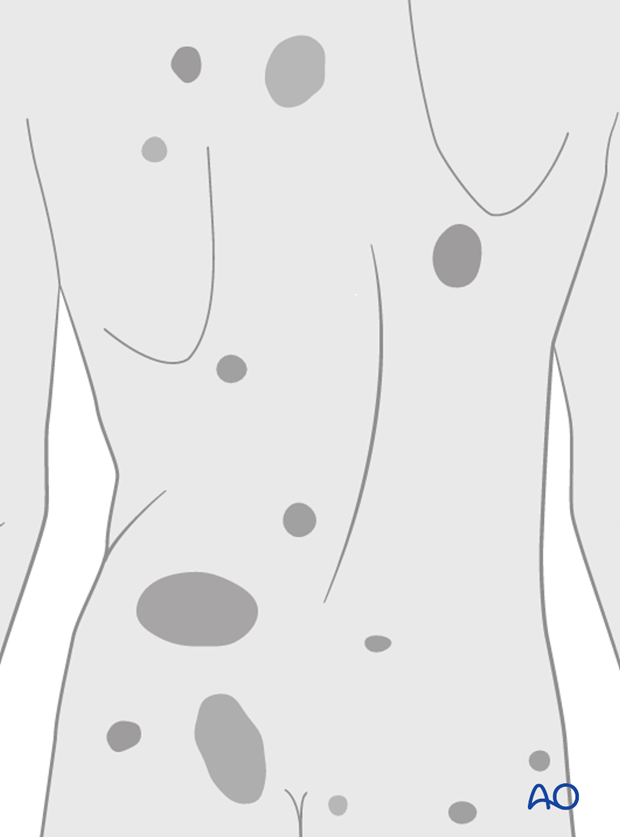
Presence of any cutaneous abnormalities
The presence of cutaneous abnormalities such as hairy spots or "café au lait" spots can be a presence of non-idiopathic types of scoliosis and should be kept in mind.
Indicators of maturity
Development of secondary sexual characteristics is a rough indication of skeletal maturity and should be kept in mind.
Gait
Gait assessment is important for indicating any possible leg length discrepancies or possible ataxia which may be an indication of spinal cord disorders.
Sensory and motor examination
Sensory and motor examination is performed in routine fashion to ensure there are no deficits or asymmetries.
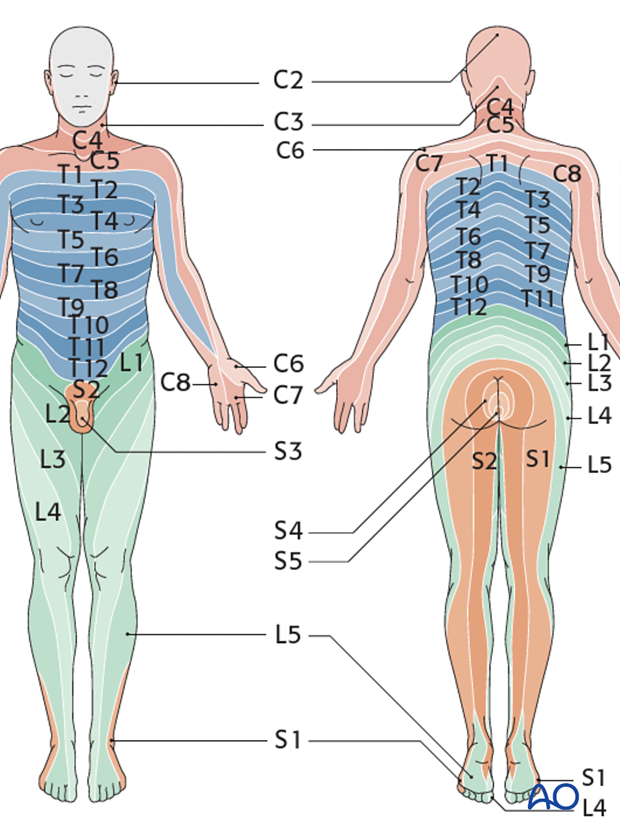
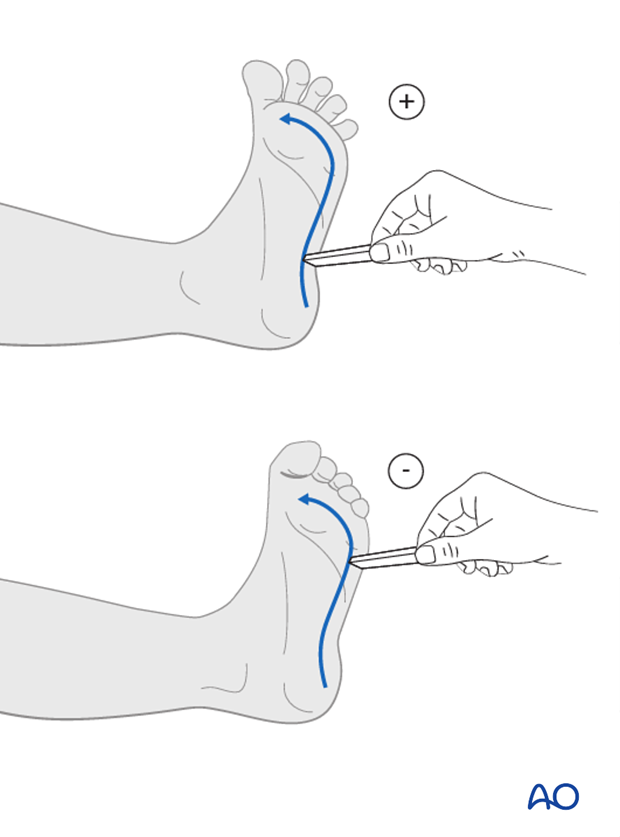
Reflex examination
Upper and lower extremities should be examined for asymmetries and deep tendon reflexes. In addition the abdominal reflex should be assessed for asymmetries as well. The presence of reflex asymmetry from side to side can be an indication of neuro axis abnormalities and may warrant further examination such as the use of MRI.
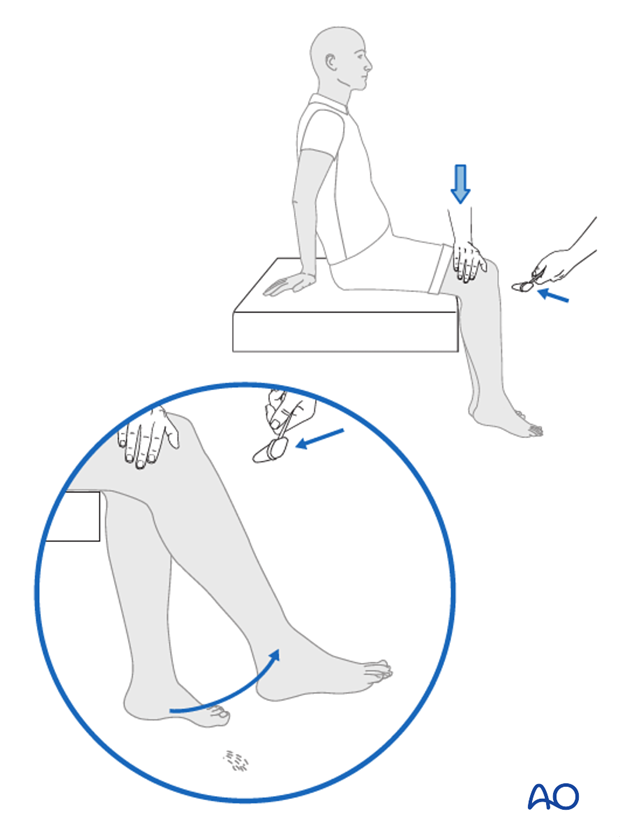
Clonus or a positive Babinski may be an indication of upper motor neuron disease or spinal cord disorders. The presence of these reflexes should warrant further examinations by MRI.
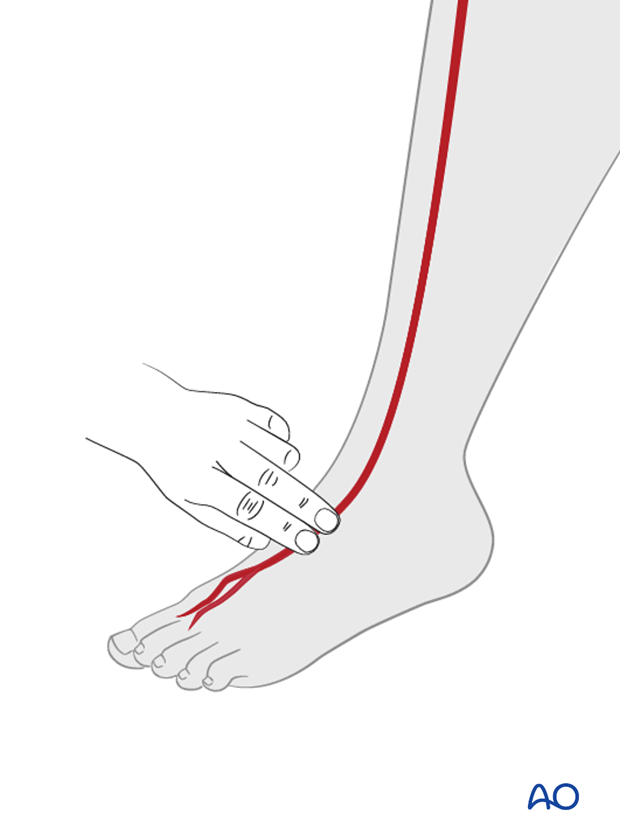
Neurovascular examination
Distal pulses are assessed to ensure adequate perfusion of all extremities.
3. Radiologic assessment
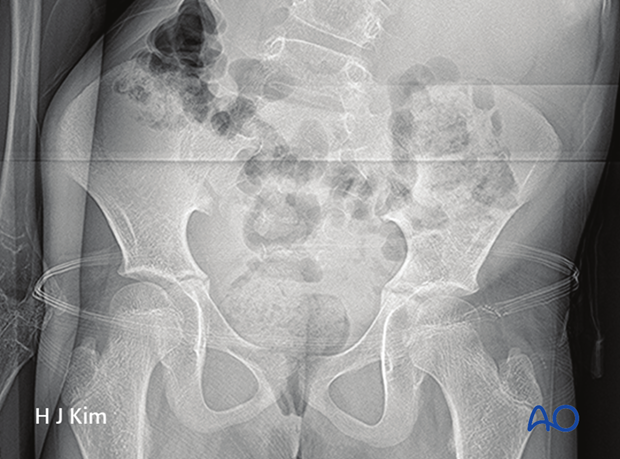
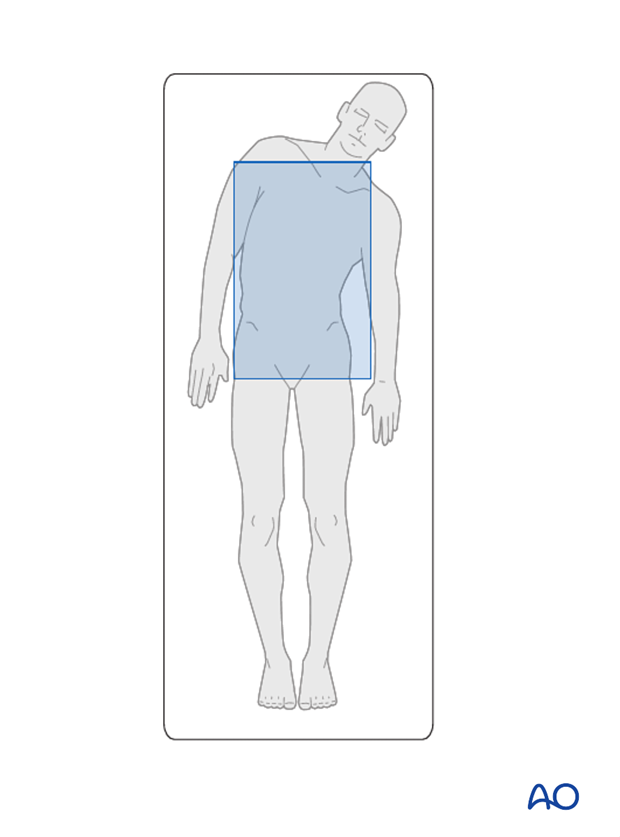
Essential radiographs
36 inch full casette standing radiographs in PA (with patient facing the film) …
...and lateral planes.
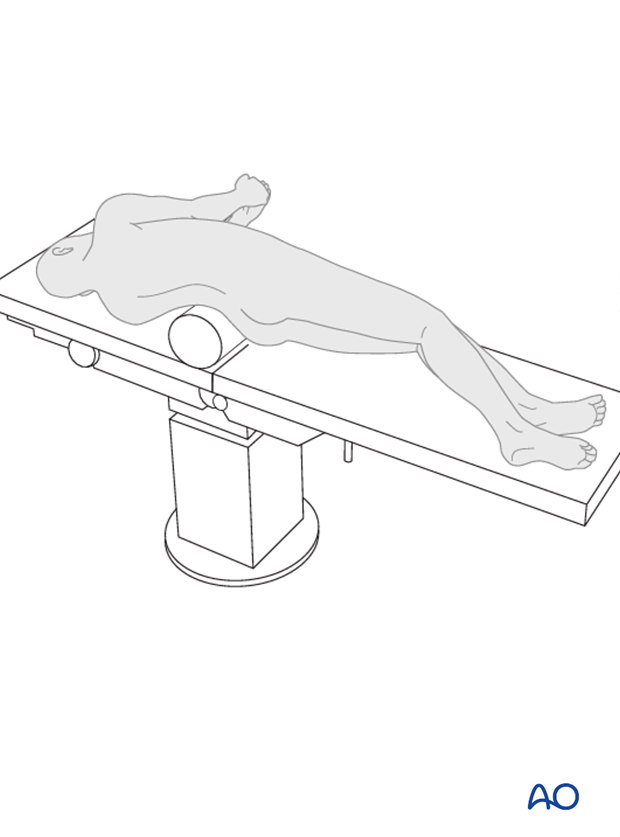
Left and right bending radiographs with the patient positioned supine.
Lumbosacral supine bending radiograph for patients with a structural lumbar curve.
Optional radiographs
Fulcrum bending radiographs. This method of flexibility assessment provides a good prediction of postoperative outcome for main thoracic curves, is highly reproducible, and can be a guide to fusion level determination.
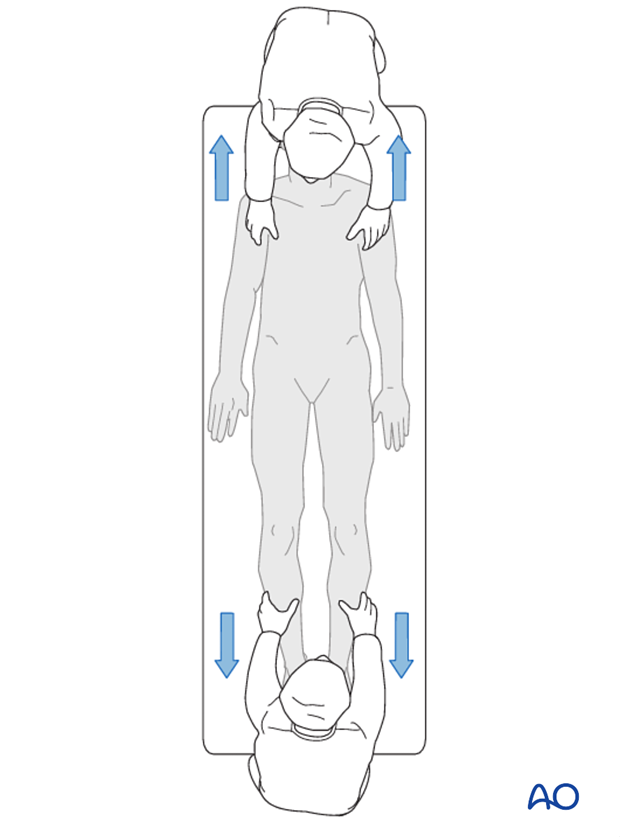
Traction radiograph under general anaesthesia. This method of flexibility assessment provides a good prediction of prediction of outcome of both thoracic and lumbar curves, and can be a guide to fusion level determination. However, it can only be carried out during surgery.
Measuring Cobb angles
In the AP view Cobb angles are measured from cranial end vertebra to caudal end vertebra. End vertebra is defined as the vertebra that is most tilted from the horizontal apical vertebra. For a given curve the cranial end plate is used for the proximal end vertebra while the caudal end-plate is used for the distal end-vertebra.
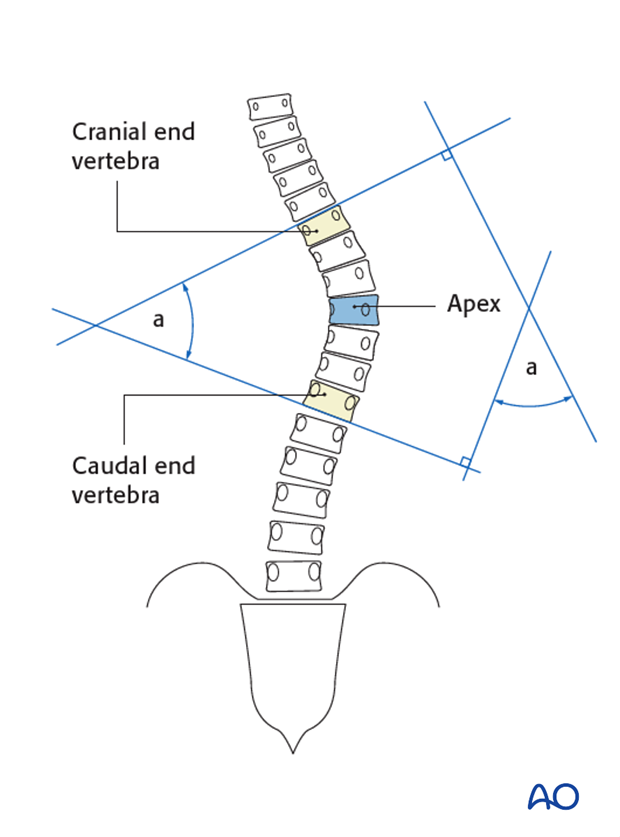
Proximal thoracic and thoracolumbar/lumbar curves should always be measured in the same manner.
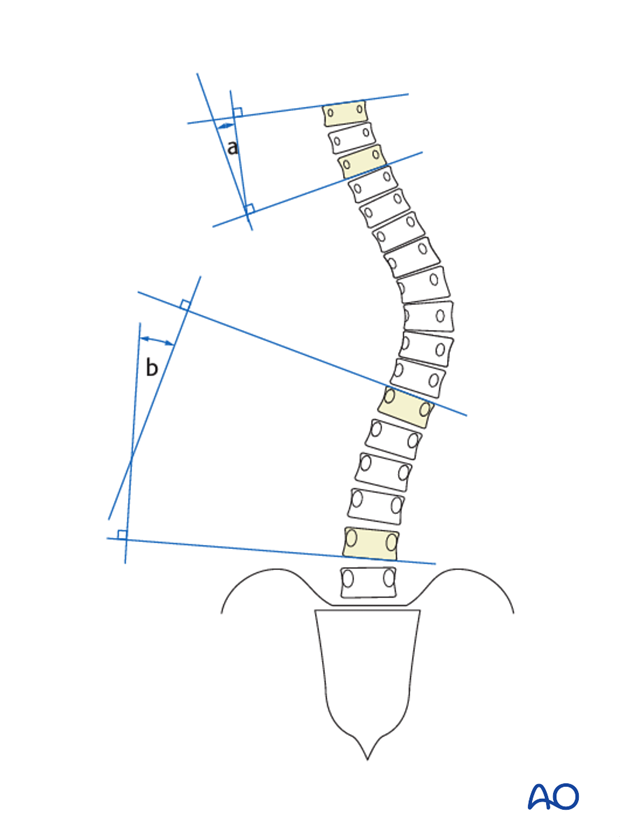
In the lateral X-ray, Cobb angles are measured in a more uniform fashion in the following way:
- A) T2-T5
- B) T5-T12
- C) T10-L2
- D) L1-S1
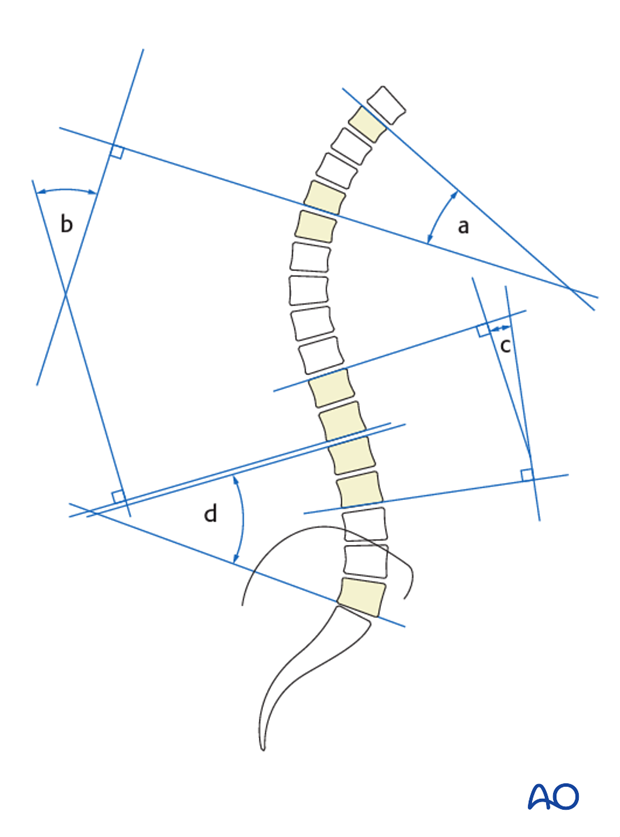
In the case of a severe kyphotic deformity an additional measurement of maximal kyphosis can be used. The superior end plate is used for the proximal end vertebra while the inferior end-plate is used for the distal end-vertebra in order to measure out the area of maximal kyphosis.
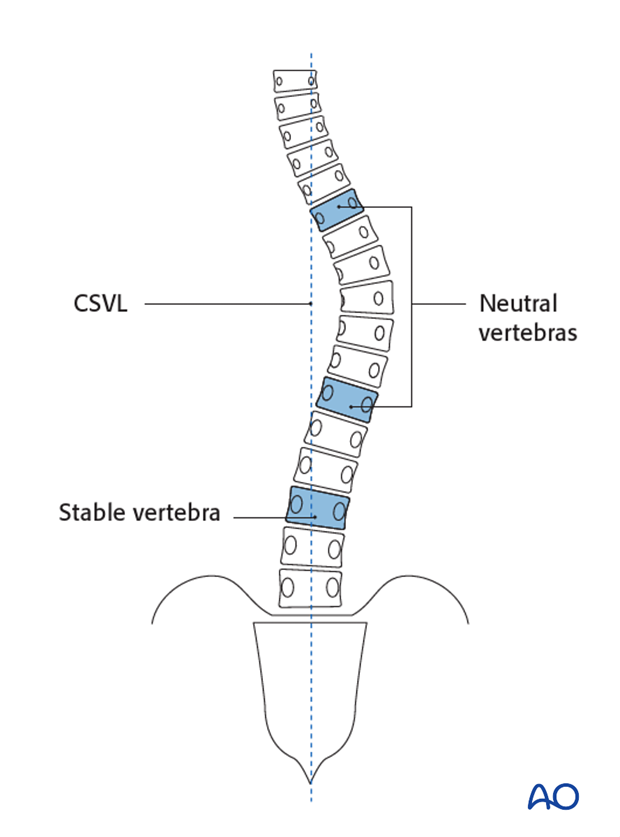
Determination of stable and neutral vertebra
Central Sacral Vertical Line (CSVL) is vertical line bisecting the sacrum.
Stable vertebra is determined by the CSVL as the most cephalad vertebra that is distal to the end vertebra that is most closely bisected by this line.
The neutral vertebra is defined as the vertebra that is not rotated. It is identified by symmetric pedicles in the coronal radiograph.
4. Radiographic markers of skeletal maturity
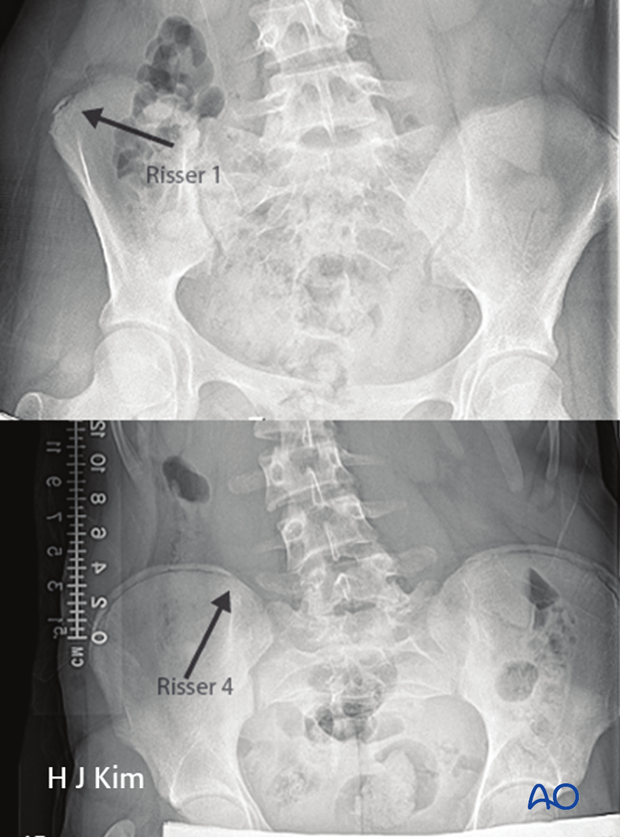
Risser sign
The Risser sign is a radiographic depiction of the iliac apophysis appearance designating skeletal maturity. It is on a 0 to 5 scale with 0 indicating skeletal immaturity and 5 indicating complete maturity.
Generally speaking peak height growth velocity occurs before the Risser sign emerge.
Triradiate cartilage
The triradiate cartilage is the acetabular apophysis which when present represents a growth period prior to the peak height velocity.
Bone age assessment
Hand X-rays can be taken to provide a good estimate of bone age. This can be used to assess time for growth remaining. Specifically attention is turned to the presence of open epiphyses at the proximal phalanx and metacarpals as well as the distal radius. If all three of these are still open, the patient most likely has more than two years of growth remaining. Closure of the distal radius epiphysis indicates skeletal maturity.

5. Generalized radiographic overview
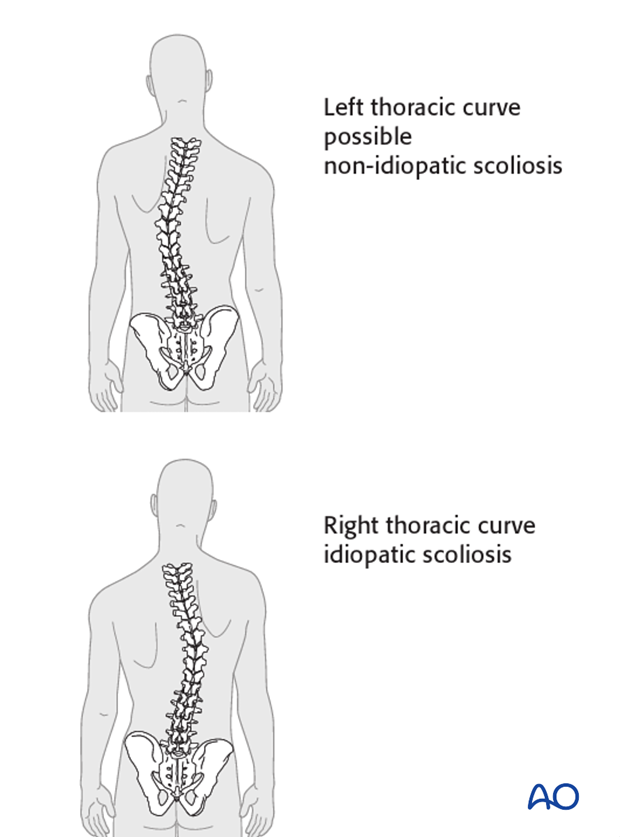
Curve directionality
Usually in idiopathic scoliosis the curve pattern is such that there is a right thoracic curve. If there is a left thoracic curve, this might be an indication of a non-idiopathic scoliosis that might necessitate further evaluation.
Shoulder balance
Shoulder balance is assessed radiographically to provide an indication for both preoperative and postoperative alignment and balance.

Pelvic obliquity
Pelvic obliquity is evaluated for its cause being due to a primary leg length discrepancy and/or from the scoliosis.