Radiological evaluation of patients with thoracolumbar trauma
1. Preliminary remarks
Radiological evaluation of an injured spine includes plain x-rays, computerized tomography (CT), and magnetic resonance imaging (MRI) scan. The purpose of radiological evaluation is to:
- Identify the location and extent of injury
- Determine features of vertebral instability
- Assess the severity of neurological compression and injury
- Classify injury patterns
- Identify multilevel injuries
2. Plain x-rays
Introduction
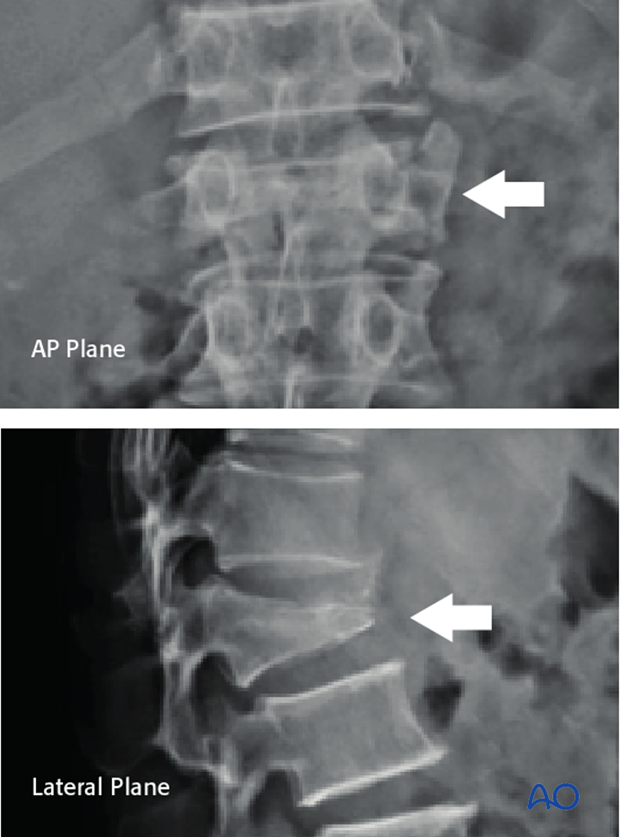
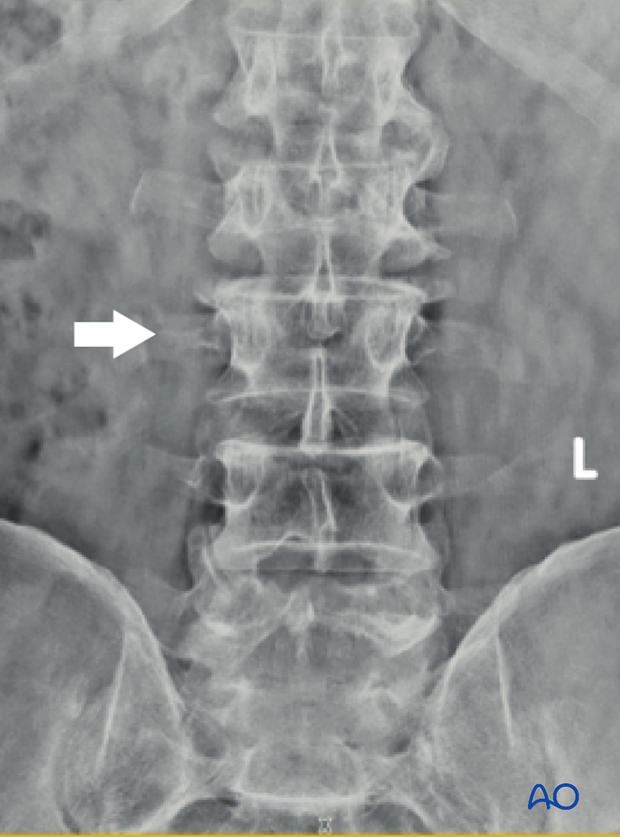
Good quality plain x-rays in two planes (antero-posterior and lateral) must be performed in all patients with suspected spinal trauma.
The appropriate x-ray is performed based on local tenderness or deformity, and the presence of neurology (in case of neurological injury).
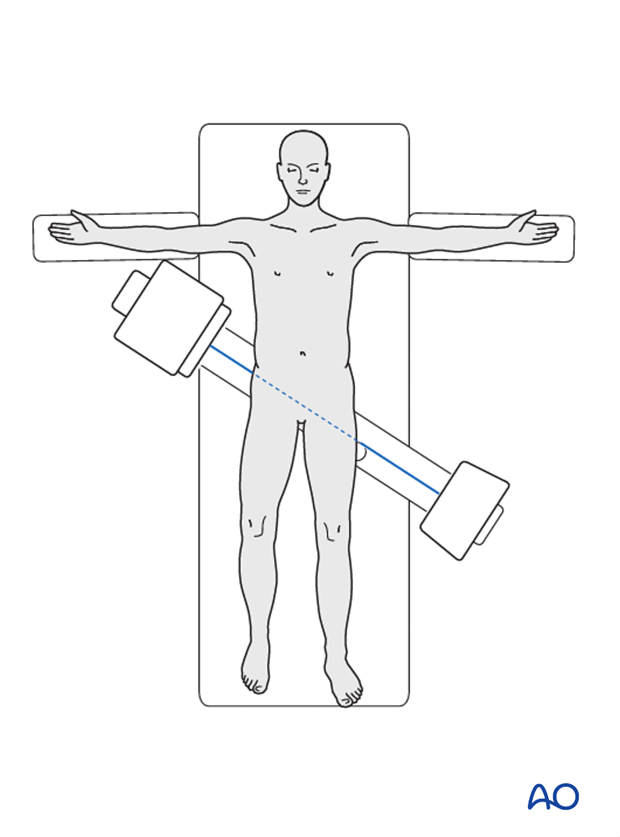
In trauma situations, it is not always possible to turn the patient, and hence a cross-table lateral view facility can be used.
It is important that the whole spine radiological survey is available to identify multilevel injury, which is present in up to 15% of patients.
Moreover, it is important to have both AP and lateral x-rays available.
If the x-rays are not satisfactory or inconclusive, a CT scan must be performed.
What is seen in the AP x-ray
In the antero-posterior film, the following factors are observed:
What is seen:
- Isolated fractures of the transverse process
What it indicates:
- A0 fracture
What is seen:
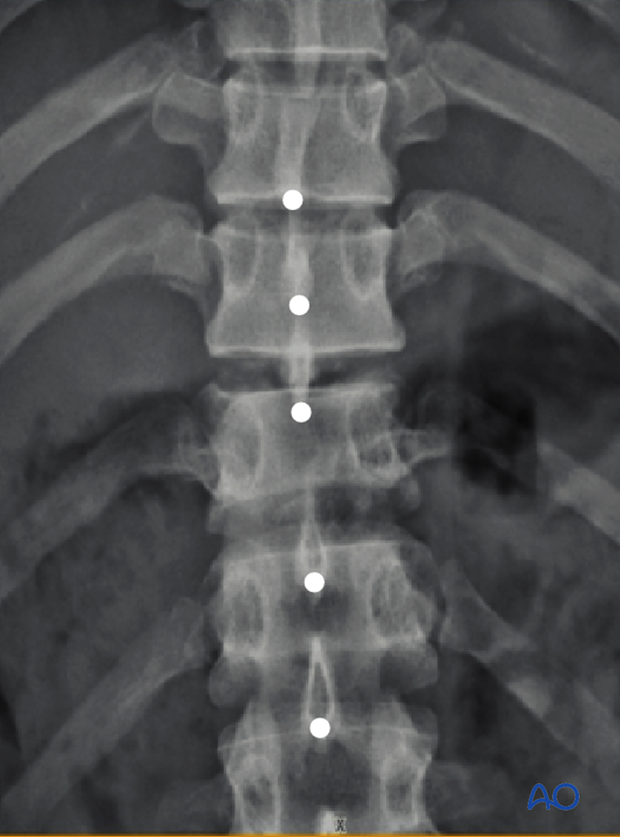
- Loss of vertebral body height (compare with the adjacent normal vertebra)
What it indicates:
- Collapse of vertebral body (A type injuries)

What is seen:
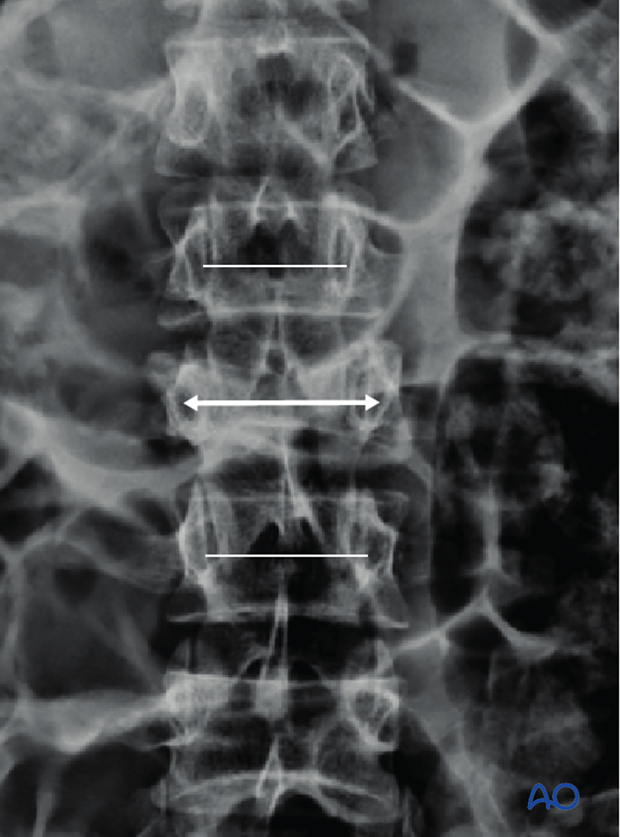
- Widening of inter-pedicular distance (Widening is identified by drawing a straight line along the medial border of the pedicles of two adjacent vertebrae)
What it indicates:
- Increase in the inter-pedicular distance indicates a burst fracture–an A3/4 injury
What is seen:
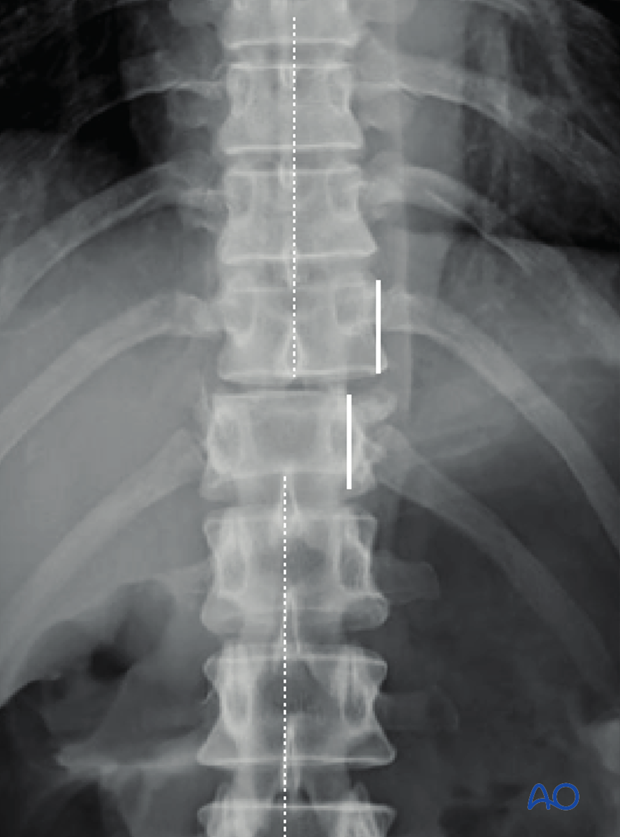
- Vertebral translation (as indicated by lateral displacement of the body or altered spinous process alignment)
What it indicates:
- C type injury
What is seen:
- Increased inter-spinous distance (compared with adjacent levels)
What it indicates:
- Distraction failure of the posterior tension band–type B injury (B1 or B2)
What is seen:
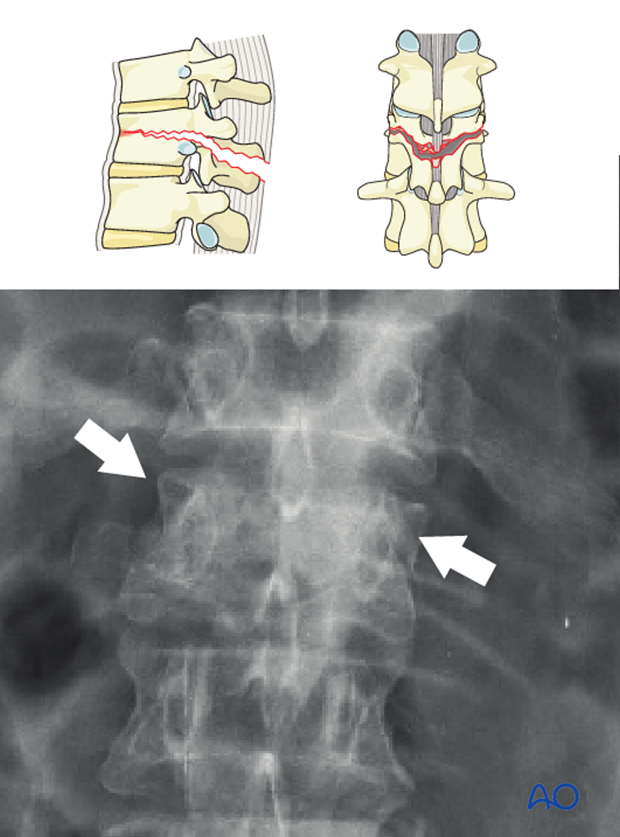
- Horizontal split in the body at the level of the pedicles
What it indicates:
- B1 injury
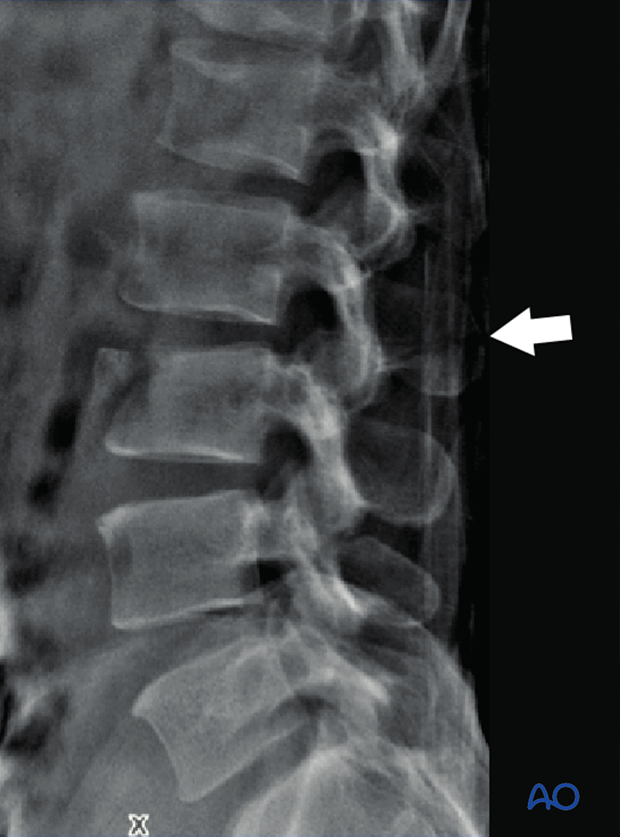
What is seen in the lateral x-rays
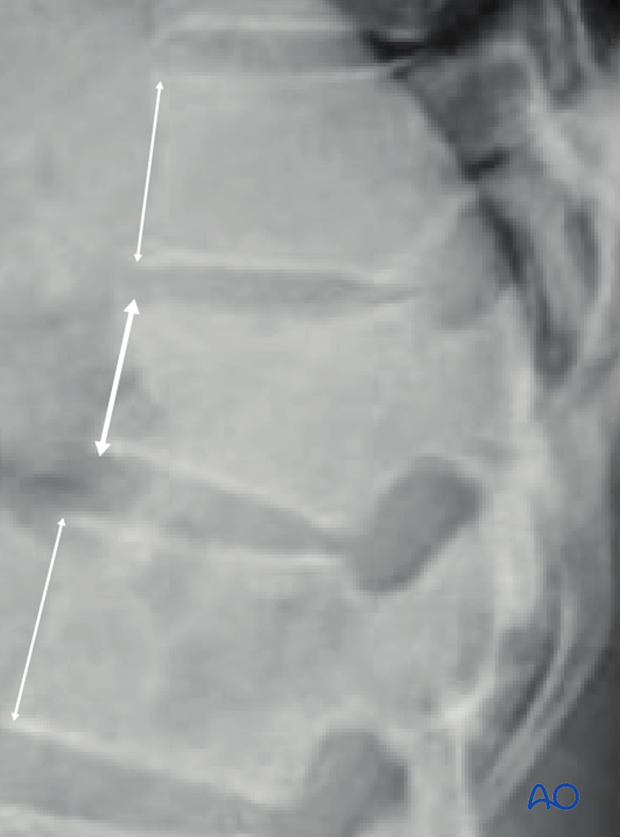
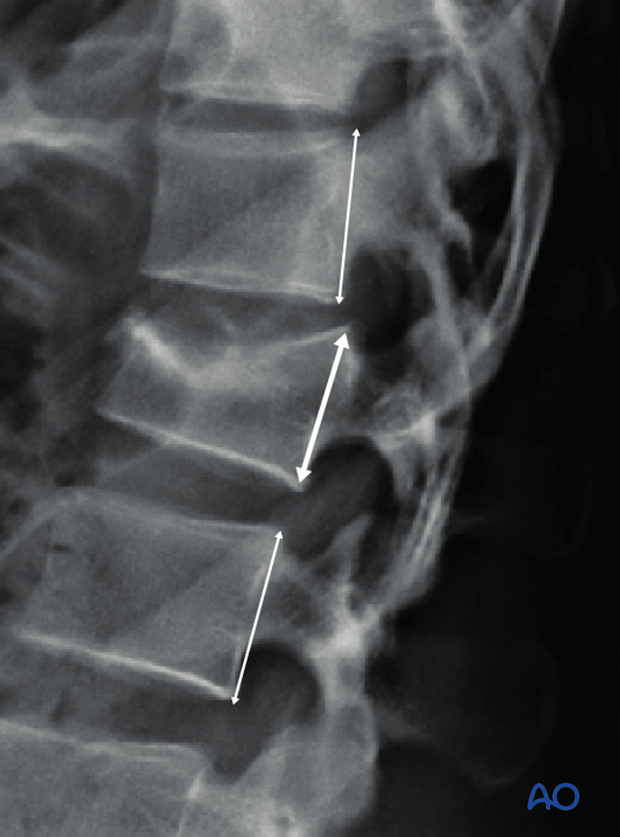
What is seen:
- Loss of anterior vertebral body height (the anterior vertebral body height is measured along the anterior vertebral border from the superior to the inferior end plate and compared to the adjacent normal vertebra)
What it indicates:
- Type A injuries
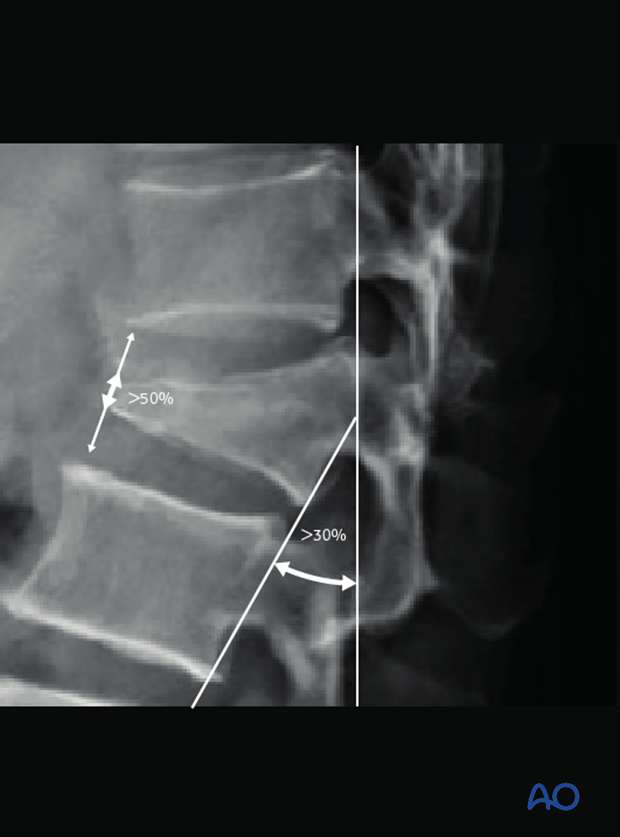
What is seen:
- Kyphosis >30 degrees and Vertebral body collapse >50%.
What it indicates:
- Type A injuries
What is seen:
- Spinous process widening
What it indicates:
- Posterior ligamentous complex injury and instability
What is seen:
- Loss of posterior vertebral body height or posterior cortical disruption (the posterior vertebral body height is measured along the posterior vertebral border from the superior to the inferior end plate and compared to the adjacent normal vertebra)
What it indicates:
- Involvement of the posterior wall of the vertebral body with possible retropulsion into the spinal canal—A3/A4 injuries.
Note: CT is indicated to assess the extent of bony injury.
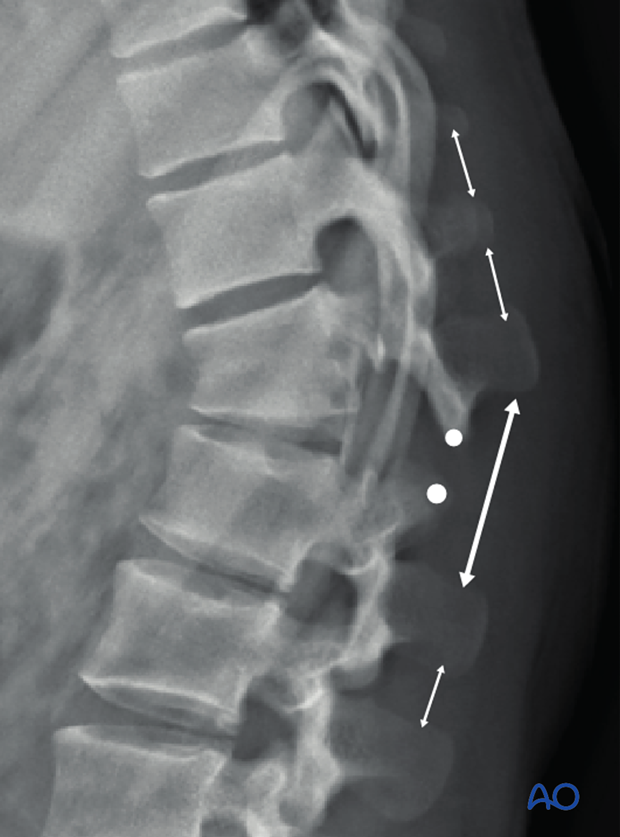
What is seen:
- Loss of spinal alignment (the presence of vertebral translation can be identified by drawing a straight line along the vertebral borders. In these situations, also look at the facet joints to look for joint subluxation or dislocation)
What it indicates:
- C type injury

What is seen:
- Separation of the facet joints with widening of the interspinous distance
What it indicates:
- B2 injury
What is seen:
- Spinous process fracture
What it indicates:
- Presence of a spinous process fracture, which may indicate just an A0 injury. However, in the presence of A1-4 injury anteriorly, a coexistent spinous process fracture would indicate a B1/2 injury. Any such suspicion would mandate further CT evaluation
- A0 or B1/2 injury
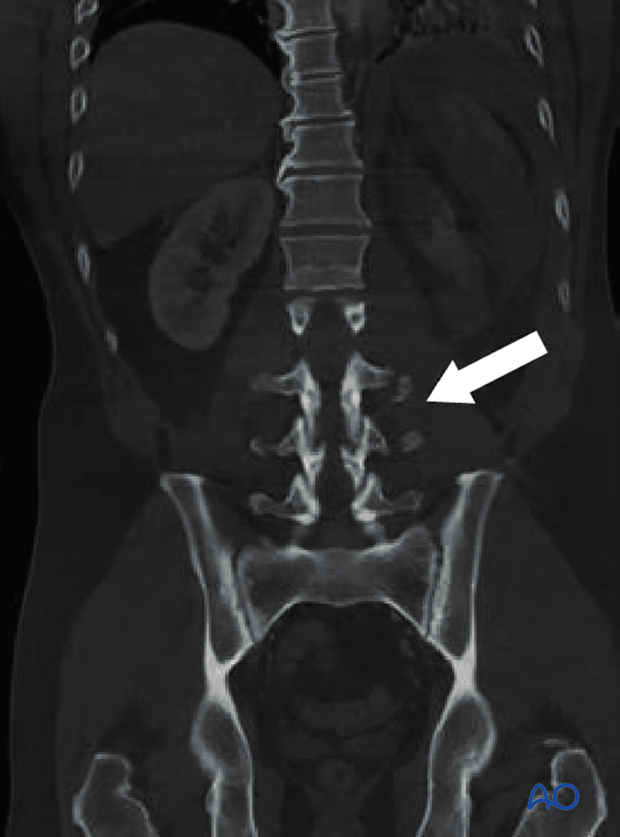
3. CT scan
Introduction
CT scans provide important details about the extent of bony injury in a patient with spinal injury. In many centers, CT is routinely performed as it reveals fractures that are not visible in plain x-rays in more than 20% of patients.
CT scans are part of the assessment for the AOSpine classification.
Advantages:
- Most accurately depicts bony injuries
- Sensitivity and specificity > 95%
- Concomitant multi-slice CT of chest, abdomen and pelvis can be done to detect visceral injuries
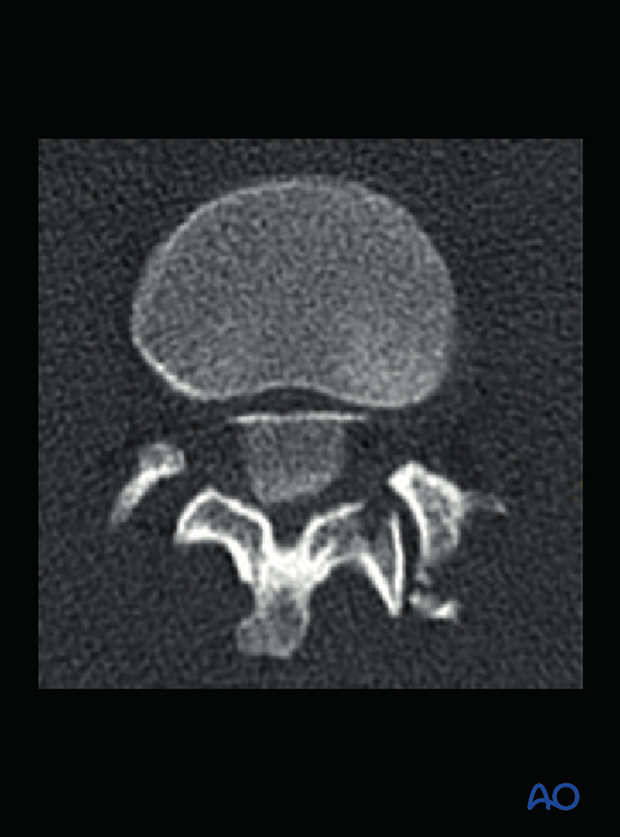
What is seen in CT scans
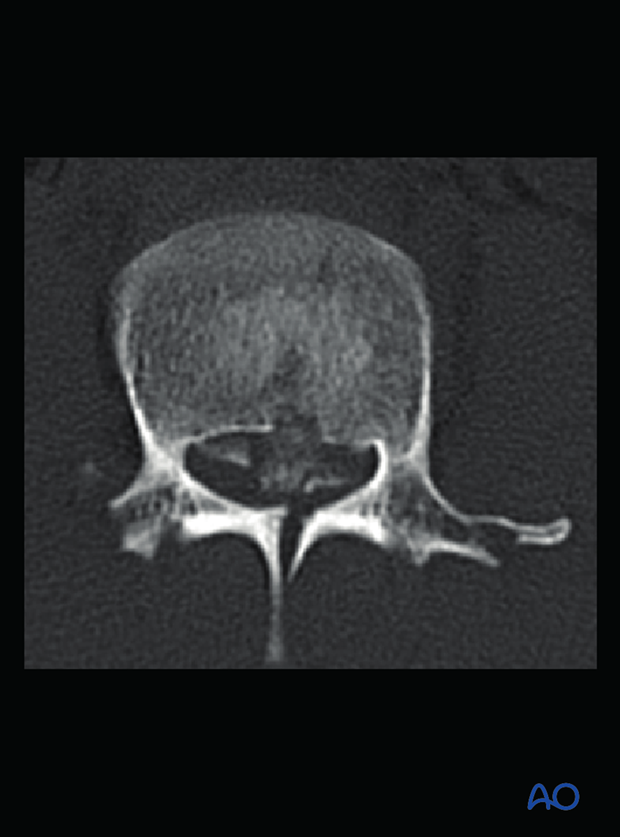
What is seen:
- Extent of vertebral body comminution (the extent of vertebral body comminution and the displacement of fragments is clearly visualised in CT images)
Which view:
- Sagittal and axial
What it indicates:
- Severity of injury
- Extent of canal encroachment
- Exact AOSpine classification
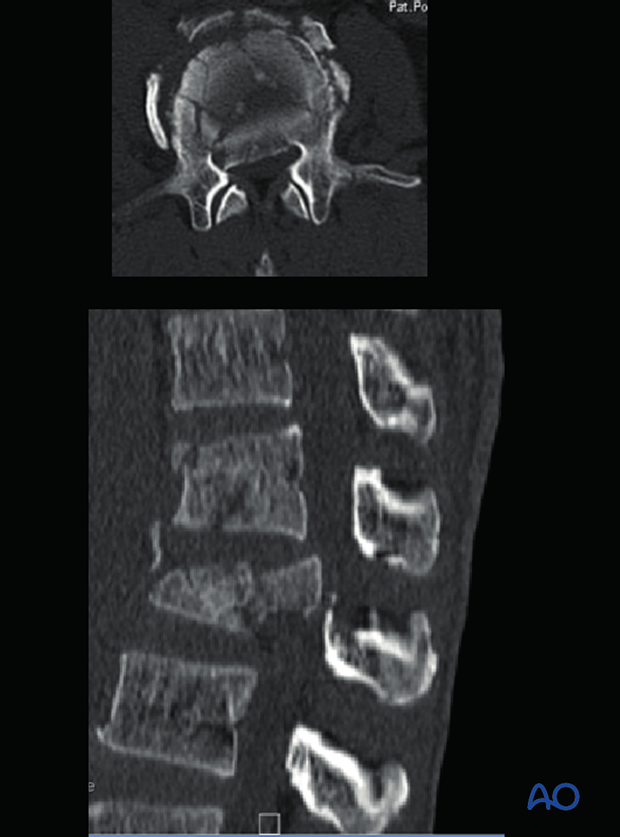
What is seen:
- Retropulsion of bone fragments (the amount and severity of retropulsion of bone fragments into the spinal canal is clearly depicted in the axial and sagittal CT images)
Which view:
- Axial and sagittal
What it indicates:
- Need for decompression when neurological damage has been detected
What is seen:
- Reverse cortical sign (the retropulsed fragment that has rotated more than 180 degrees so that the cortical surface is opposed to the cancellous surface of the main vertebral body)
Which view:
- Axial
What it indicates:
- Severe disruption of the posterior ligamentous complex
- Due to 180° rotation the fragment will not unite with the main vertebral body
- Anterior decompression is usually preferred
- Contraindication for ligamentotaxis
What is seen:
- Lamina fracture
Which view:
- Coronal and axial
What it indicates:
- Eventual dural and nerve root entrapment
Note : Caution should be exercised during exposure to avoid inadvertent dural tear and neural injury.
What is seen:
- Pedicle fracture
Which view:
- Axial and sagittal
What it indicates:
- Instability
- Need to avoid pedicle screw fixation at this level
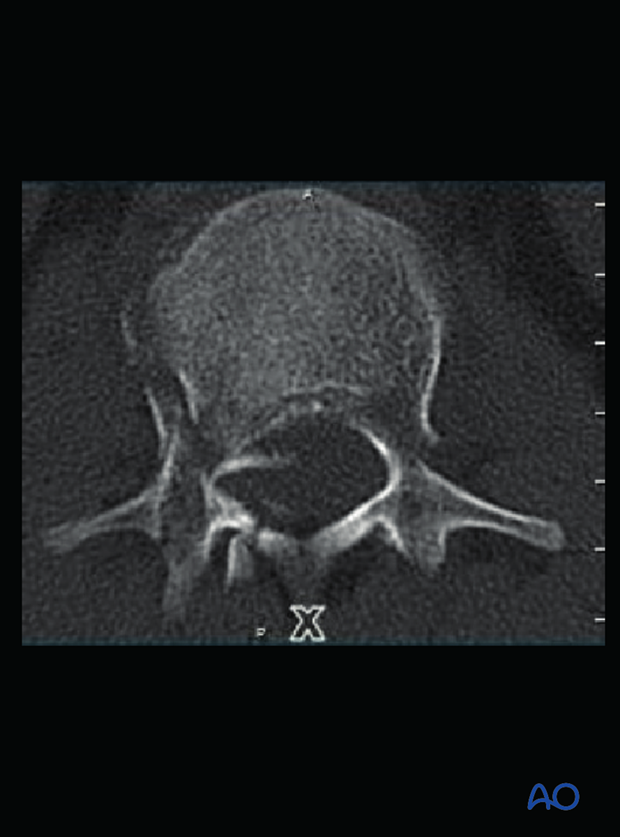
What is seen:
- Spinous process fracture
Which view:
- Sagittal
What it indicates:
- Instability—B1/2 injury
Note: Presence of an isolated vertical spinous process fracture may indicate just A0 injury. However in the presence of A1-4 injury anteriorly, a co-existent spinous process fracture would indicate a B1/2 injury.

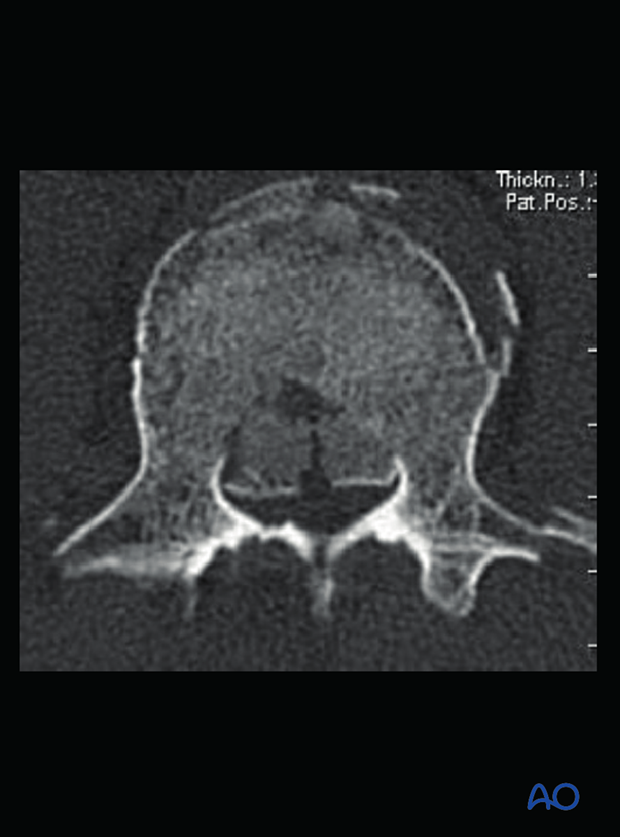
4. MRI scan
Introduction
MRI scans give useful information about the extent of soft tissue injury that has occurred during the spinal injury. However the availability and longer time spent in the console precludes its regular use in all spinal trauma patients, especially in polytraumatized patients and those with hemodynamic instability.
Indications:
- Patients with neurological deficit
- Patients with suspicious PLC injury
Advantages:
- In patients with neurological deficit, MRI accurately depicts the extent of cord compression, edema, hemorrhage and the presence of cord transection.
- Determines extent of injury to posterior ligamentous complex
- Identifies damage to discoligamentous complex
- Helps to identify multi-level non-contiguous injuries
Disadvantages:
- Cost and availability
- Delay in definitive management
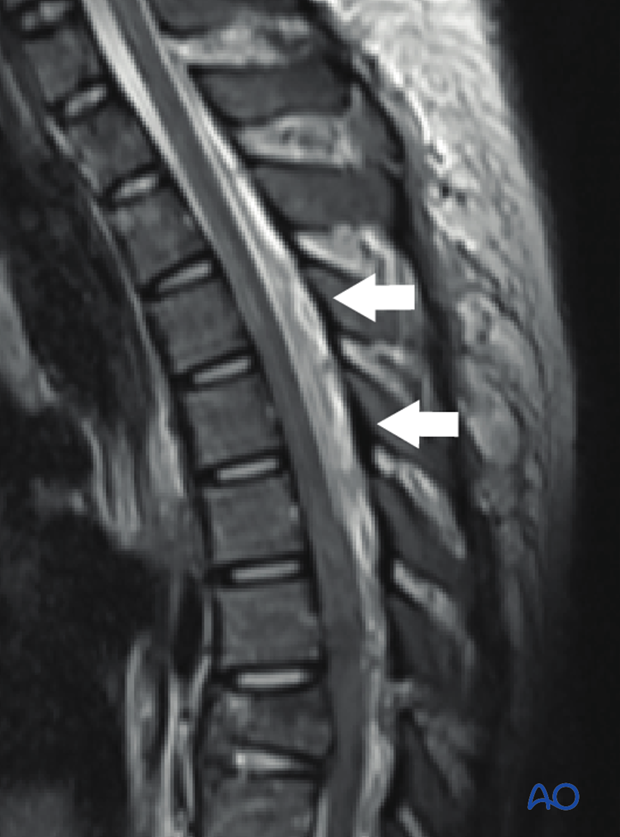
What is seen:
- Bony compression of spinal cord
What it indicates:
- Need for decompression, posterior or anterior
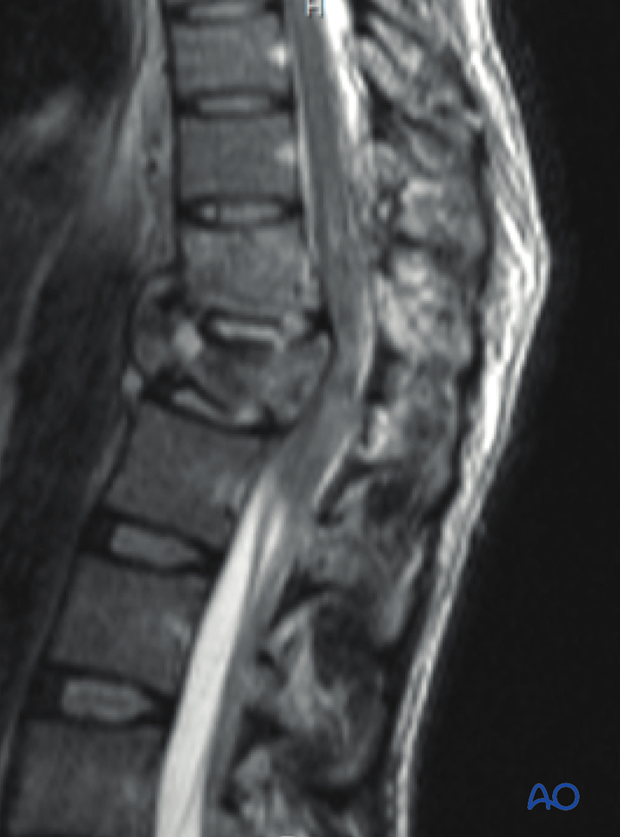
What is seen:
- Hyperintense signal changes in cord
What it indicates:
- Cord injury
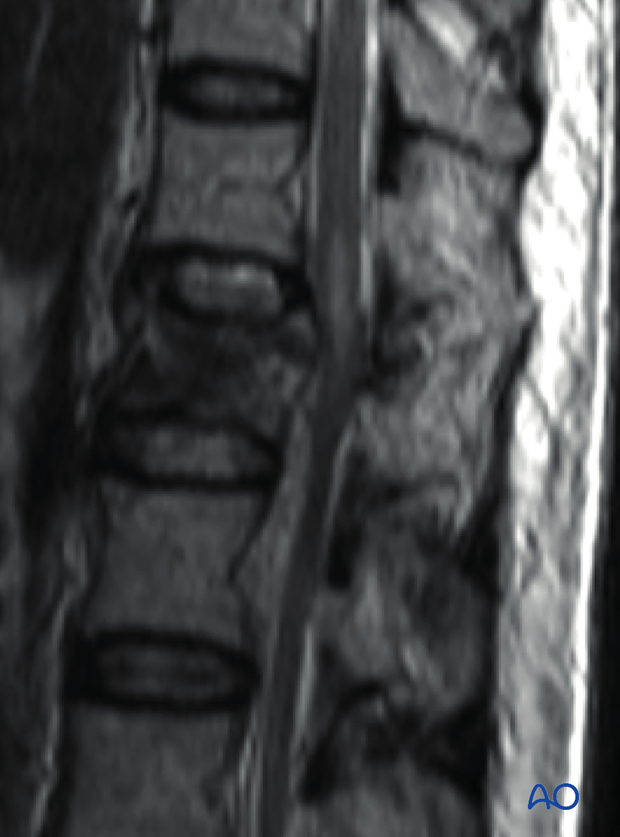
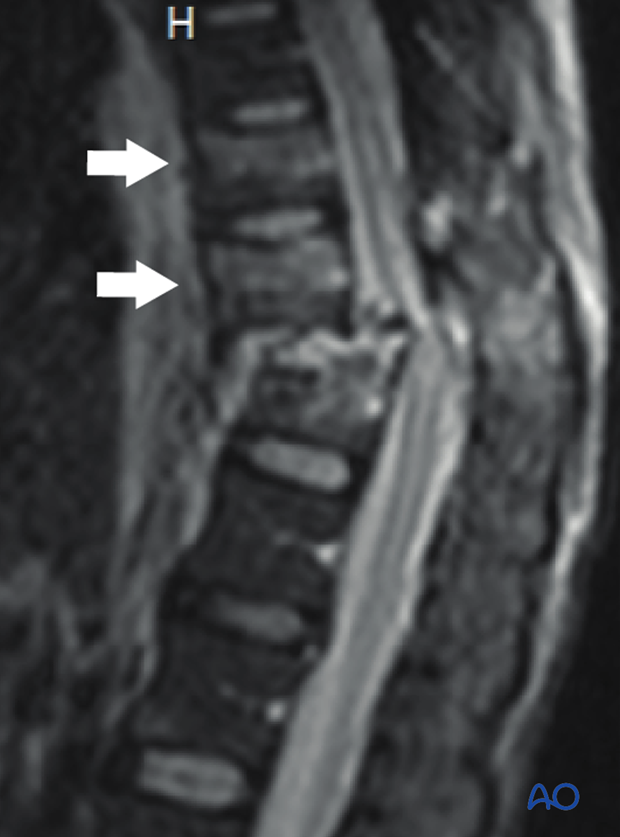
What is seen:
- Hyperintense signal in the PLC
What it indicates:
- Loss of integrity of PLC
Note : Fat suppressed images show hyperintense signal changes in the PLC better indicating disruption of PLC.
What is seen:
- Marrow edema in adjacent bones
What it indicates:
- Subtle injury of adjacent segments
What is seen:
- Epidural hematoma
What it indicates
- Extensive injury
What is seen:
- Cord transection
What it indicates:
- No chance for neural recovery

What is seen:
- Multilevel injury
What it indicates:
- May require multilevel intervention













