Complications with mandible fractures
1. General considerations
The most common complications from mandibular fractures are:
- Bleeding
- Nerve damage
- Nonunion
- Sequestrum formation
- Osteomyelitis
- Malunion with malocclusion
2. Bleeding
Oral bleeding can occur from initial trauma due to sharp bone edges, during surgical approach or fracture manipulation, or by incorrect placement of implants.
Hemostasis via ligation is the preferred method. Electrocautery should be avoided.
If bleeding cannot be stopped, carotid artery ligation can be used.
3. Nerve damage
Nerve damage can occur from initial trauma due to sharp bone edges, during surgical approach or fracture manipulation or by incorrect placement of implants.
4. Nonunion
Nonunion is the result of biological and/or mechanical errors that interfere with the bone healing process.
As a result of the trauma, the vascular supply to the bone may be poor. Improper handling of the soft tissues, inadequate surgical technique and unstable fracture fixation can lead to mandibular nonunion.
The presence of periodontal disease at the fracture site predisposes the bone to nonunion and infection.
5. Osteomyelitis and sequestrum formation
Osteomyelitis with sequestrum formation in mandibular fractures occur in:
- Open fractures
- Patients with periodontal disease at the fracture site
- Poor fracture stability from poor selection of implants or conservative management of the fracture
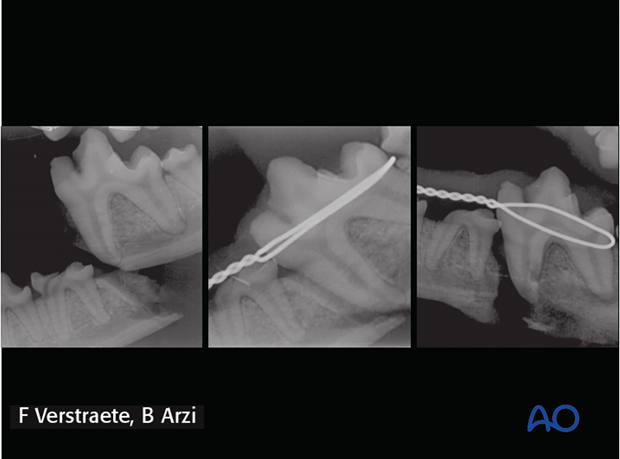
Right mandibular fracture and sequestrum formation in a dog.

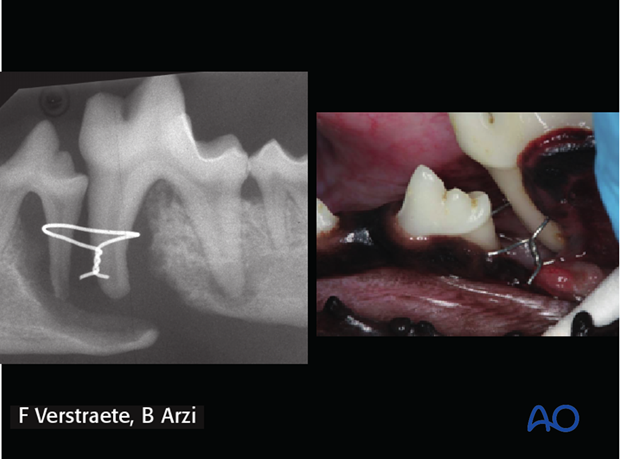
Intraoral approach for soft tissue debridement and removal of a sequestrum.

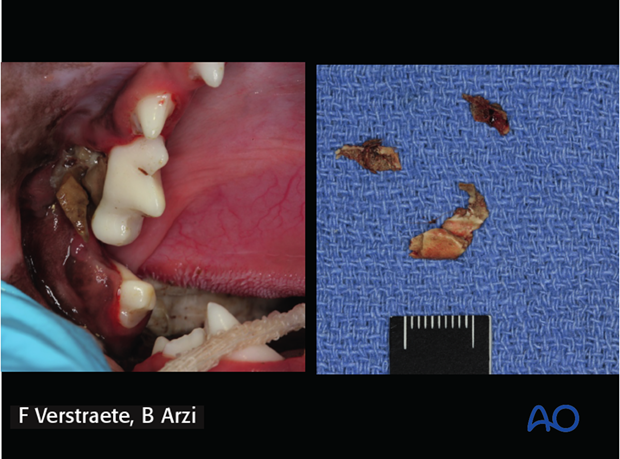
Soft tissue closure using the intraoral approach.

6. Malunion with malocclusion
Malunion can occur due to inappropriate alignment of the fracture segments and inappropriate fixation (poor implant selection or conservative management).
7. Temporomandibular joint (TMJ) ankylosis
Definition
TMJ ankylosis is an abnormal fusion of the mandibular head of the condylar process and the mandibular fossa of the squamous temporal bone. It is a possible sequela of oral and maxillofacial fractures.
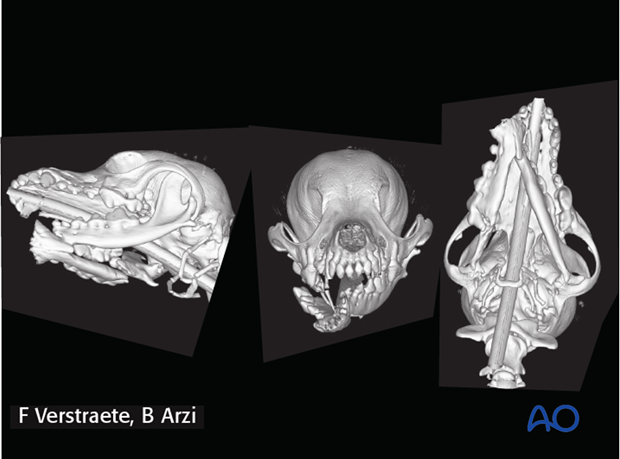
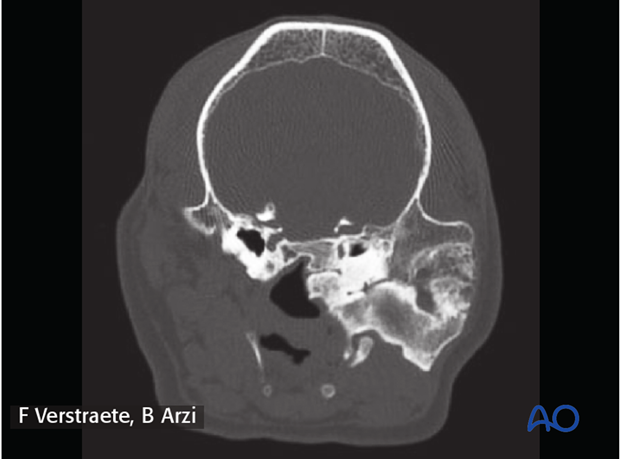
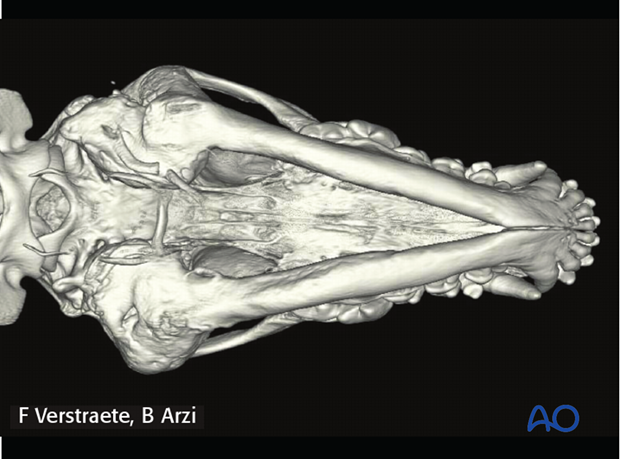
The picture shows a unilateral TMJ ankylosis in a dog. The bone fusion involves the entire TMJ and including the base of the skull.
If the bony fusion is extraarticular, such as between the zygomatic arch and the coronoid process of the mandible, the term ‘false’ or ‘pseudoankylosis’ may be used.
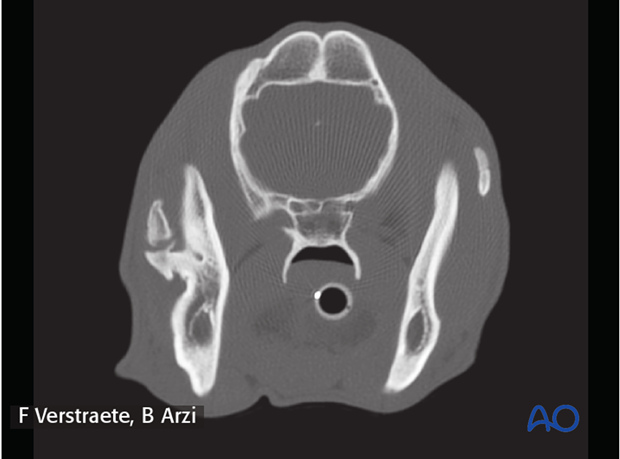
The picture shows a unilateral pseudoankylosis in a dog following a maxillofacial trauma. Note the bone fusion of the coronoid process and the zygomatic arch.
TMJ ankylosis or pseudoankylosis may occur at any age but is seen most commonly following maxillofacial trauma that occurred at a young age. When present during skeletal development, ankyloses may impair facial growth and development.
Clinical signs
- Gradual inability to open the mouth
- Mandibular drift towards the affected side of the mandible
- Complete immobilization of the mandibles with no ability to open the mouth.
The picture shows a bilateral TMJ ankylosis in a 1.5-year-old dog following maxillofacial trauma. Note that the jaws are completely locked closed and the dog is unable to open the mouth.

Imaging
Diagnosis of TMJ ankyloses and pseudoankylosis is performed using computed tomography (CT) or cone beam CT (CBCT). Skull radiographs have a poor diagnostic yield for diagnosis of TMJ ankylosis and pseudoankylosis because of the structural configuration of the skull.
Treatment
Treatment is achievable only through surgical resection of the ankylosis or pseudoankylosis with therapy to prevent recurrence. Surgical osteoplasty of the TMJ or the pseudoankylosis is aimed at removal of excessive fibrous and/or bony tissues. Gap arthroplasty (removal of a bone wedge to create a gap) is recommended over condylectomy to reduce the incidence of recurrence, especially in young dogs and cats.












