Clinical evaluation of patients with thoracolumbar trauma
1. Primary survey
The primary survey consists of the ABCDE scheme. This means that Airway, Breathing, Cardiovascular Status, Disability, Exposure and Environmental Control are checked.
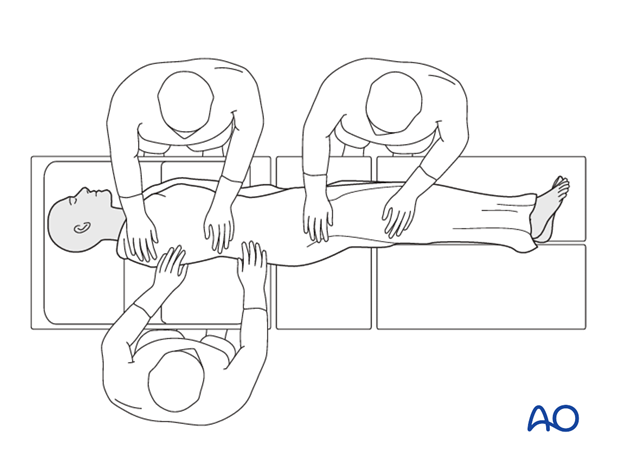
With a suspected cervical spine injury, the cervical spine should be immobilized in a hard collar. A cervical spine injury should be suspected in anyone with impaired level of consciousness, with a high velocity injury, or in anyone with a spine fracture. If a spine board was used for transport, the patient should be logrolled and the spine board removed (after ABC have been established). This maneuver can be incorporated into the physical examination of the spine.
2. Airway assessment
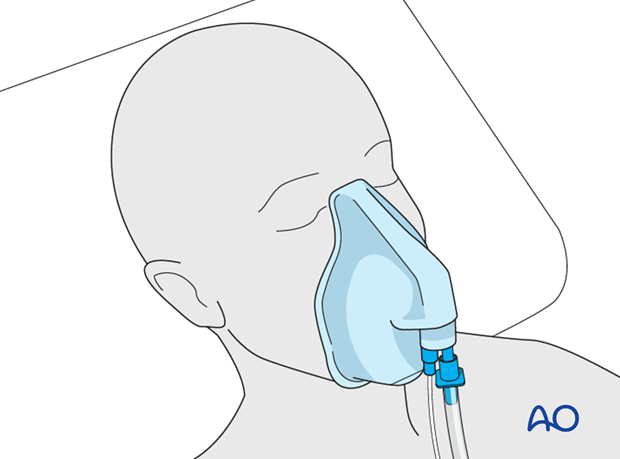
In the assessment of the airway it should be determined whether the patient can breathe and talk freely. The patient should be placed on oxygen by face mask or nasal prongs.
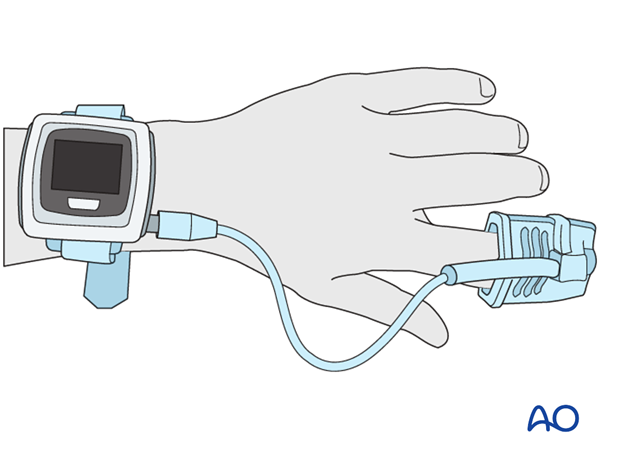
An oxygen monitor is put on a finger to measure oxygen tension.
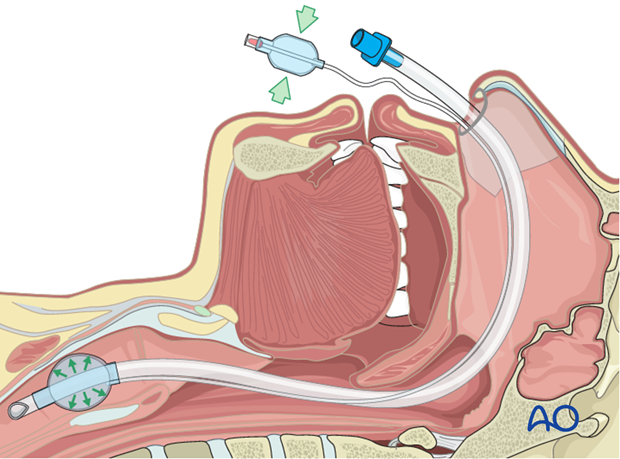
If a cervical spine injury is suspected, and the airway is compromised, an awake fiberoptic intubation is the preferred technique to establish an airway. As an alternative, conventional orotracheal intubation can be used with manual inline attraction applied. With significant facial trauma, a cricothyroidotomy should be considered. If undertaken, the cricothyroidotomy should be converted to a formal tracheostomy in the operating room.
If the airway is secure, see next step.
3. Breathing assessment
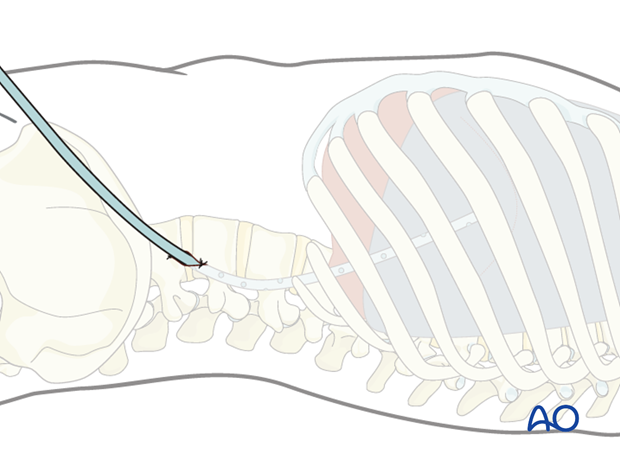
Breathing is assessed by observing adequate movement of the chest. With a cervical spinal cord or high thoracic cord injury, bedside spirometry can be helpful. A vital capacity of less than one liter is concerning and may warrant intubation and mechanical ventilation.
If ribs are fractured, the movement will be paradoxical.
If breathing is not normal, artificial ventilation, decompression, and drainage of tension pneumothorax/hemothorax and closure of open chest injury, if present, are performed.
If breathing is secure, see next step.
4. Cardiovascular status
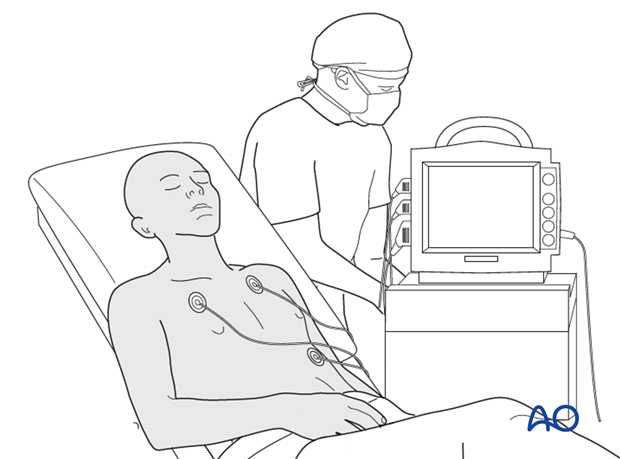
The patient should be hooked up to a cardiac monitor. An arterial line should be established to monitor blood pressure and to obtain arterial blood gases.
With a spinal cord injury it is critical to maintain the mean arterial blood pressure over 85 mm Hg. It is important to distinguish neurogenic from hypovolemic shock. Neurogenic shock occurs with a severe cervical or high thoracic spinal cord injury and is characterized by hypotension, low heart rate, and well perfused extremities. Hypovolemic shock should be suspected with polytrauma and abdominal, pelvic, or severe orthopedic injuries. Hypovolemic shock is associated with hypotension, rapid heart rate, and cool extremities.
Neurogenic shock should be treated with an initial bolus of 1l of crystalloid or colloid solution. Following this, if hypotension persists, an inotrope (dopamine or levophed) infusion should be initiated. Hypovolemic shock should be treated as per usual protocol with appropriate volume resuscitation.
If irregularities are observed, an infusion should be prepared and external bleeding is stopped, if present. In some cases, medication to increase blood pressure or heart beat has to be used.
If cardiovascular status is adequate, see next step.
5. Disability
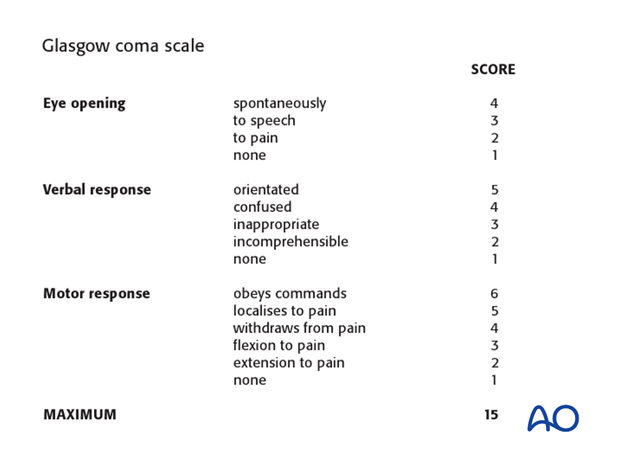
Basic neurological assessment is carried out. Level of consciousness should be assessed using the Glasgow coma score.
Impairment in level of consciousness can cloud the accuracy of the neurological assessment of the limbs.
An abbreviated neurological assessment of the extremities should be undertaken as part of the primary survey. A more detailed neurological assessment according to the ASIA standards is part of the secondary survey.
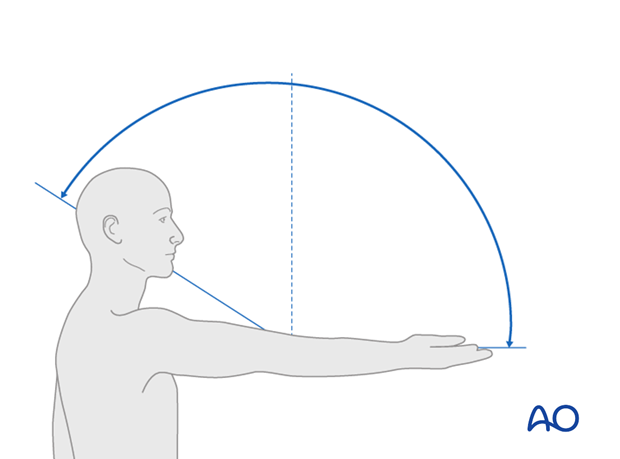
The abbreviated neurological assessment should include asking the patient to elevate both forelimbs, assessment of biceps and triceps function, wrist extension, and wrist flexion and grip strength.
In the lower extremities, hip flexor function, knee extension and flexion, and ankle dorsiflexion and plantar flexion should be assessed.
The sensory assessment should be part of the secondary survey.
In cases of unconscious patients, spinal injuries are easily missed or misunderstood. CT scans of the head and the entire spine have to be checked.
6. Exposure and environmental control
Undress the patient and check for visible injuries. Examine the extremities for any injuries and assess the circulatory status.
After the primary survey is completed, the initial set of imaging studies is typically undertaken.












